This study’s object was to reveal the attitudes toward the preimplantation genetic testing (PGT) for Hereditary Breast and Ovarian Cancer (HBOC) in the reproductive age lay public and the genetic professionals. The subjects of this survey were the individuals with/without history of breast and/or ovarian cancer and the clinical genetic professionals. A web-based anonymous questionnaire survey was conducted. 425 laypeople and 149 genetic professionals answered. Of the genetic professionals, 36% had been asked about reproductive options for HBOC from their clients. More than half of the laypeople (55.1-61.9%) considered PGT to be acceptable. But about half of the clinical genetic professionals (50.1%) considered it to be unacceptable and about thirty percent of the clinical geneticists considered PGT for HBOC to be acceptable for the reason of client’s Autonomy. After the European Society of Human Reproduction and Embryology (ESHRE) ethics taskforce approved PGT for adult onset and multifactorial diseases in 2003, PGT for adult-onset HBOC has become a general reproductive option. However, in Japan, the academic societies don’t allow PGT for hereditary cancer. It may be necessary to discuss whether PGT for HBOC would be allowed and support systems to aid reproductive decision making for younger couples should be urgently discussed in Japan.
Decision Making; Genetic Counseling; HBOC; Preimplantation Genetic Testing; Reproduction.
Abbreviations
PGT: Preimplantation Genetic Testing
HBOC: Hereditary Breast and Ovarian Cancer
BRCA1/2: BRCA1 or BRCA2
PND: Prenatal Diagnosis with the Intention of Termination of Pregnancy
The prevalence of breast cancer in Japan in 2021 was estimated to be approximately 95,000, with about 15,700 deaths due to breast cancer during that year. These numbers continue to rise every year and it is estimated that the number of people with breast cancer after 10 years will exceed 110,000. (Cancer statistics in Japan, 2021). Five to ten percent of breast cancer is considered to be hereditary, among which hereditary breast and ovarian cancer (HBOC) caused by a BRCA1 or BRCA2 (BRCA1/2) gene mutation is the most common. Women with a BRCA1/2 gene mutation has been recommended taking breast MRI, risk-reducing mastectomy (RRM) and/or risk reducing bilateral salpingo-oophorectomy (RRSO).
In 2018, the BRCA1/2 genetic testing was covered by health insurance system as a companion diagnostic test for PARP inhibitor treatment for recurrent metastatic breast cancer in Japan. Since April 2020, the targeted patients of the testing have been expanded to breast cancer, ovarian cancer, prostate cancer, and pancreatic cancer patients, with suspected HBOC. For the breast and/or ovarian patients with a BRCA1/2 mutation, the annual breast MRI, RRM, and RRSO became covered by the public health insurance system. While expanding the testing leads to increase the cancer patients who will benefit from the medical management, it might cause that patients will face to the reproductive issues and their younger family members will unexpectedly realize that they are at-risk of HBOC. Some literatures raised the reproductive issues related to the BRCA1/2 mutation carriage. Twenty percent of 77 BRCA1/2 carriers thought that they would decide not to have children [1] and about 21.5% of 163 women who were un-partnered felt more pressure to get married and 41% of 284 women whose families were not complete reported that carrier status impacted their decision to have biological children [2]. Also, in Japan, about half of young women hesitated to get married and have children, assuming that "if I were a BRCA1/2 mutation carrier" [3]. Therefore, BRCA1/2 genetic information has the potential to negatively affect the marriage and reproductive decision making of younger people.
Reproductive genetic testing options for individuals with a BRCA1/2 mutation include Prenatal Diagnosis with the intention of termination of pregnancy (PND) and Preimplantation Genetic Testing for Monogenic (PGT-M). With regard to reproductive decision-making among hereditary breast cancer patients and families, awareness and attitudes toward the use of PND and PGT-M have been investigated. PND is physically and emotionally challenging [4] and the use of PGT-M raises ethical concerns given the reduced penetrance, its adult-onset and the availability of preventive and therapeutic options [5]. On the other hand, for PGT-M, a physically demanding in vitro fertilization/intracytoplasmic sperm injection (IVF/ICSI) treatment is necessary regardless of the couple's fertility.
The requirements for PND in Japan and those for PGT-M are prescribed by the “Guidelines for Genetic Testing” (Aug 2003) published by genetic medicine-related associations and “Views/Bylaws on Pre-Implantation Testing for the Serious Hereditary Diseases” (revised in Jan 2022) published by the Japan Society of Obstetrics and Gynecology, respectively. Although the severity or seriousness of the disease has been extremely important in the requirements, the term “serious” had not been clearly defined for a long time. At last, it was clarified in the new guidance. The definition of seriousness of disease is below: "In principle, before reaching adulthood, the symptoms that strongly impair daily life or that their survival is jeopardized appear, and in order to avoid them, there is currently no effective treatment or the advanced, or highly invasive treatment are required." An adult-onset hereditary disease such as HBOC does not fall under the definition of “serious disease,” and PND or PGT-M is never presented as a normal option during genetic counseling in Japan. However, looking outside of Japan, the European Society of Human Reproduction and Embryology (ESHRE) ethics taskforce argued that PGT-M was acceptable for adult onset and multifactorial diseases, despite uncertainties about prospective improvements in preventive and therapeutic options in 2003 [6]. As a result, nowadays, PGT for HBOC has been allowed and it became to be one of the reproductive options in the countries such as the United Kingdom, the Netherlands and the United States [2, 7, 8].
With the increase of BRCA1/2 genetic testing for cancer patients, it is expected that the reproductive age family members at-risk of HBOC would face the decision-making problems related to marriage and reproduction. Outside of Japan, the option of PGT for HBOC are provided in general but it has not been allowed by the academic society in Japan. However, it is important to reveal the attitudes towards the reproductive option among public people and clinical genetic professionals so as to discuss the issues of reproductive option for not only HBOC but also hereditary cancer and adult-onset hereditary diseases.
Subjects
The subjects of this survey were 1) the healthy individuals with no history of cancer, 2) the breast and/or ovarian cancer patients, and 3) the clinical genetic professionals. The healthy individuals and the cancer patients were reproductive age that was 20 to 49 years old. The clinical genetic professionals were the Japanese board-certified instructors of clinical geneticists and the certified genetic counselors, both of which are certified by the Japan Society of Human Genetics and the Japanese Society for Genetic Counseling. The clinical geneticists with unknown address were excluded when sending a survey request letter.
Survey Design and Questionnaire
We conducted a web-based anonymous questionnaire survey for all subjects. The surveys were conducted from September 2019 to March 2020. Informed consent was obtained from all respondents before answering the questionnaire. This study was approved by the Medical Research Ethics Committee of Tokyo Medical and Dental University (the approval numbers were M2019-016 for the survey of the certified genetic counselors, M2019-108 for the survey of the healthy individuals and cancer patients and M2019-308 for the survey of the clinical geneticists).
In this survey the subjects were asked to answer whether they consider PND and PGT for HBOC to be acceptable as a reproductive option. The questionnaire for the healthy people and the cancer patients contained the demographic features such as sex, age, educational background, status of marriage, the experience of pregnancy/childbirth, the experience of conducting of PND for the chromosomal aneuploidies, and household income. The questionnaire for the genetic professionals contained the items as sex, age range, the experience of pregnancy/childbirth, the experience of genetic counseling for HBOC, the experience of being asked about PND or PGT for HBOC from their patients or clients. In the question about the experience of pregnancy/childbirth, male respondents were asked to answer about their partner or wife. Furthermore, the questionnaire for the clinical geneticists included the item about the reason for their opinion which is acceptability of PND and PGT for HBOC. The following options were presented as the reasons: 1) to respect the client's Autonomy, 2) because HBOC is an adult-onset disease, 3) because HBOC is an “actionable” disease, 4) because there is a possibility that treatment and prevention for HBOC reduce quality of life (QOL) and body image, 5) because HBOC is not a “serious” disease, 6) because HBOC has a wide range of phenotype, 7) because the penetration rate is not 100%, 8) because PND is a test that considers abortion of pregnancy/because PGT is performed for fertilized eggs before pregnancy, 9) because it’s OK if the criteria for implementation (genetic counseling system, approval by the clinical ethics committee, etc.) are met 10) because it's too early to discuss this issue, 11) because there is no legal system for genetic discrimination in Japan, 12) because academic societies do not approve PND/PGT for HBOC at this time, 13) other. The multiple choices were allowed.
Statistical Analysis
The frequency distribution and response rate were investigated in each question. The Chi-square test and the residual analysis were used to analysis the comparison of the groups. And the Bonferroni correction was used to counteract the problem of multiple comparisons. In the laypeople the relationship between the acceptability of PND and PGT for HBOC and the characteristic of the respondents, such as age, household income and final education, was analyzed by using the Pearson's correlation coefficient (r). In the correlation analyses, answers obtained using the scales, such as the acceptability of PND and PGT for HBOC (2: acceptable, 1: neither, 0: unacceptable), household income (5: over 1200, 4: 800 to <1200, 3: 400 to <800, 2: 200 to <400, 1: under 200) and final education (5: graduate school, 4: university, 3: college/vocational school, 2: high school, 1: junior high school), were regarded as evenly spaced numerical values. The relationship between the acceptability of PND and PGT for HBOC and the experience of pregnancies (“yes” or “non”) was analyzed by using the Chi-square test. The statistical significance level was set at p<.05. Statistical analysis was performed using SPSS Statistics, Version 23.0. (Armonk, NY, IBM Corp).
Subjects
Participants were 425 laypeople and 149 genetic professionals for this study. The study included 218 healthy individuals with no history of cancer and 207 breast and/or ovarian cancer patients, as well as 63 certified genetic counselors and 86 clinical geneticists. The response rates were 25.1% (63/251) in the certified genetic counselors and 29.4% (86/293) in the clinical geneticists. Characteristic data of the respondents are shown in Table 1.
Table 1. Characteristic data of the respondents
|
Healthy Individuals |
Cancer Patient |
Genetic Professionals |
|
(N=218) |
(N=207) |
(N=149) |
Sex |
|
|
|
|
|
|
Male |
109 |
(50.0%) |
15 |
(7.2%) |
66 |
(44.3%) |
Female |
109 |
(50.0%) |
192 |
(92.8%) |
75 |
(50.3%) |
N.A. |
0 |
|
0 |
|
8 |
(5.4%) |
Age (years old) |
|
|
|
|
|
|
20-29 |
72 |
(33.0%) |
16 |
(7.7%) |
14 |
(9.4%) |
30-39 |
74 |
(34.0%) |
67 |
(32.4%) |
22 |
(14.8%) |
40-49 |
72 |
(33.0%) |
124 |
(59.9%) |
38 |
(25.5%) |
50-59 |
- |
|
- |
|
45 |
(30.2%) |
60-69 |
- |
|
- |
|
27 |
(18.1%) |
Over 70 |
- |
|
- |
|
3 |
(2.0%) |
Experience of pregnancy |
|
|
|
|
|
|
I have |
72 |
(33.0%) |
118 |
(57.0%) |
102 |
(68.5%) |
None |
146 |
(67.0%) |
89 |
(43.0%) |
38 |
(25.5%) |
N.A. |
0 |
|
0 |
|
9 |
(6.0%) |
Household income (ten thousand yen) |
|
|
|
|
|
|
Under 200 |
11 |
(5.0%) |
15 |
(7.2%) |
- |
|
200 to <400 |
50 |
(22.9%) |
33 |
(15.9%) |
- |
|
400 to <800 |
73 |
(33.5%) |
67 |
(32.4%) |
- |
|
800 to <1200 |
31 |
(14.2%) |
29 |
(14.0%) |
- |
|
Over 1200 |
12 |
(5.5%) |
19 |
(9.2%) |
- |
|
N.A. |
41 |
(18.8%) |
44 |
(21.3%) |
- |
|
Final education |
|
|
|
|
|
|
Junior high school |
5 |
(2.3%) |
5 |
(2.4%) |
- |
|
High school |
56 |
(25.7%) |
55 |
(26.6%) |
- |
|
College/vocational school |
41 |
(18.8%) |
69 |
(33.3%) |
- |
|
University |
83 |
(38.1%) |
62 |
(30.0%) |
- |
|
Graduate school |
28 |
(12.8%) |
9 |
(4.3%) |
- |
|
N.A. |
5 |
(2.3%) |
7 |
(3.4%) |
- |
|
N.A: Not Available
The mean ages of the laypeople were 34.6 years old in the healthy group and 40.6 years old in the patient group (t-test: p=.003). About PND for chromosomal aneuploidies, 42 healthy individuals (19.3%) and 38 patients (18.4%) knew it well (Chi-square test: n.s.) and 128 healthy individuals (58.7%) and 113 patients (54.6%) knew it a little (Chi-square test: n.s.). Of the laypeople with a history of pregnancy, 8 healthy individuals (11.1%) and 27 patients (22.9%) performed the PND for aneuploidies (Chi-square test: p<.01) and 15 healthy individuals (20.8%) and 19 patients (16.1%) had considered conducting it, but did not (Chi-square test: n.s.).
Of the 141 genetic professionals, 127 (85.2%) provided genetic counseling related to HBOC. Of the 127 professionals, 46 (36.2%) had been asked about PND or PGT for HBOC from their patients or clients.
Attitudes toward PND and PGT for HBOC
Responses to the questions about attitudes toward PND and PGT for HBOC are shown in Table 2.
Table 2. Attitudes for prenatal diagnosis and pre-implantation genetic testing for HBOC
|
Healthy individuals |
Cancer patients |
Genetic professionals |
All (N=218) |
History of pregnancy |
All (N=207) |
History of pregnancy |
All (N=149) |
History of pregnancy |
Yes (n=72) |
Non (n=146) |
Yes (n=118) |
Non (n=89) |
Yes (n=102) |
Non (n=38) |
Prenatal diagnosis |
Acceptable |
134 (61.5%) |
50 (69.4%) |
84 (57.5%) |
97 (46.9%) |
51 (43.2%) |
46 (51.7%) |
20 (13.4%) |
13 (12.7%) |
4 (10.5%) |
Unacceptable |
35 (16.1%) |
8 (11.1%) |
27 (18.5%) |
16 (7.7%) |
6 (5.1%) |
10 (11.2%) |
92 (61.7%) |
64 (62.8%) |
26 (68.4%) |
Neither |
49 (22.5%) |
14 (19.4%) |
35 (24.0%) |
94 (45.4%) |
61 (51.7%) |
33 (37.1%) |
37 (24.8%) |
25 (24.5%) |
8 (21.1%) |
Chi-square test |
- |
n.s. (p=.20) |
- |
n.s. (p=.06) |
- |
n.s. (p=.10) |
Pre-implantation genetic testing |
Acceptable |
135 (61.9%) |
49 (69.0%) |
86 (58.9%) |
114 (55.1%) |
60 (50.8%) |
54 (60.7%) |
46 (30.9%) |
30 (29.4%) |
11 (28.9%) |
Unacceptable |
31 (14.2%) |
7 (9.9%) |
24 (16.4%) |
15 (7.2%) |
8 (6.8%) |
7 (7.9%) |
75 (50.3%) |
53 (52.0%) |
21 (55.3%) |
Neither |
52 (23.9%) |
16 (21.1%) |
36 (24.7%) |
78 (37.7%) |
50 (42.4%) |
28 (31.5%) |
28 (18.8%) |
19 (18.6%) |
6 (15.8%) |
Chi-square test |
- |
n.s. (p=.29) |
- |
n.s. (p=.28) |
- |
n.s. (p=.28) |
n.s: not significance
The ratio of respondents that considered PND and PGT for HBOC to be acceptable as a reproductive option was highest in healthy group (PND: 61.5%, PGT: 61.9%), whereas the ratio that considered those to be unacceptable was highest in the professional group (PND: 61.7%, PGT: 50.3%). About 40% of cancer patients chose “neither” in the acceptability of PND and PGT (45.4%, 37.7%, respectively). It was found that there was a significant difference in the attitude toward PND and PGT for HBOC among the three groups (Chi-square test: p<.01). The residual analysis showed that there were significantly more people who considered PND and PGT for HBOC to be acceptable in the healthy group, that there were significantly more people who considered those to be neither in the patient group (p<.01) and that there were significantly more people who considered those to be unacceptable in the professional group (p<.01). In the professional group, there were significantly more people who considered PGT for HBOC to be acceptable than those who considered PND for HBOC to be acceptable (PGT: 30.9%, PND: 13.4%; Chi-square test: p<.01). A similar tendency was observed in the patient group, but the difference was not significant (PGT: 55.1%, PND: 46.9%; Chi-square test: n.s.).
In the healthy group, the demographic features, such as age, household income and final education, were not significantly related with attitudes toward PND for HBOC (age r=.043, household income r=.017, education r=-.032) and PGT for HBOC (r=.044, r=.048, r=-.112, respectively). In the also cancer patient group, the relationships between the demographic features and the attitudes toward PND and PGT for HBOC were not shown (PND: r=.032, r=-.009, r=-.049; PGT: r=.032, r=.025, r=.048, respectively). The experience of pregnancy was not related to the attitudes forward PND and PGT for HBOC in each group (shown in Table 2). However, in the whole laypeople as healthy people and cancer patients the ratio of people who considered PND for HBOC to be unacceptable was significantly higher in those who had no history of pregnancy (n=37, 15.7%) than in those who had a history of pregnancy (n=14, 7.4%, p<.01). The significant difference between laypeople who had no history of pregnancy and who had history of pregnancy was not shown in the acceptability of PGT for HBOC.
The ratio of the genetic professionals who considered PGT as a “life/survival-related choice” (64.4%) was significantly higher than the ratio of both healthy individuals (43.6%, p<.01) and cancer patients (43.0%, p<.01) (Table 3).
Table 3. Answers about whether pre-implantation genetic testing is “life-related choices”
|
Healthy individuals |
Cancer patients |
Genetic professionals |
(N=218) |
(N=207) |
(N=149) |
Yes |
95 |
(43.6%) |
89 |
(43.0%) |
96 |
(64.4%) |
No |
43 |
(19.7%) |
39 |
(18.8%) |
41 |
(27.5%) |
Neither |
80 |
(36.7%) |
79 |
(38.2%) |
12 |
(8.1%) |
Respondents’ Reasons for Their Answers to Acceptable/Unacceptable for PND and PGT
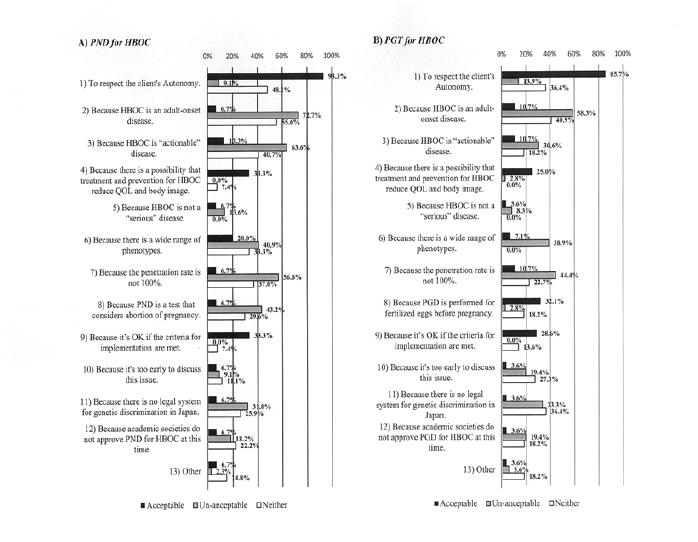
Of the 86 clinical geneticists, 17.4% (n=15) considered PND for HBOC to be acceptable, 51.2% (n=44) considered it to be unacceptable, and 31.4% (n=27) could not determine either acceptable or un acceptable. Moreover, 32.6% (n=28) of the clinical geneticists considered PGT for HBOC to be acceptable 31.9% (n=36) considered it to be unacceptable, and 25.6% (n=22) could not determine either acceptable or unacceptable. The reasons of their answers were shown in Figure 1.
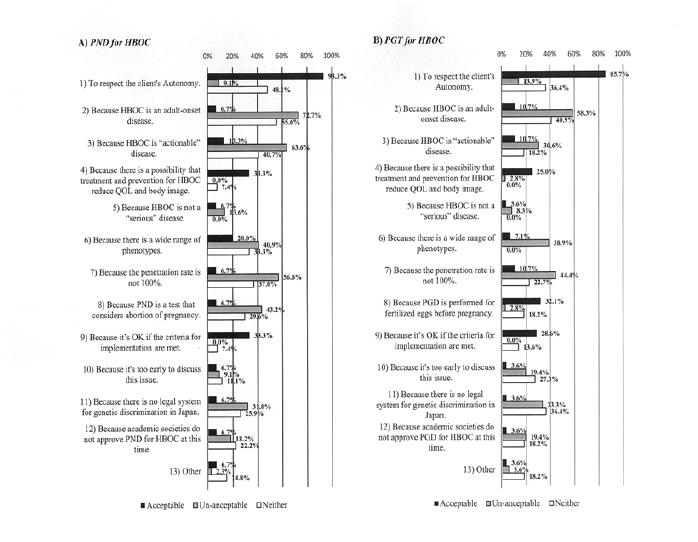
Figure 1: Clinical geneticists’ attitudes and mindsets towards PND and PGT for HBOC
The reasons to answer PND for HBOC to be acceptable/unacceptable/neither (A) and the reasons to answer PGT for HBOC to be acceptable/unacceptable/neither (B). A black bar shows the answer from the clinical geneticists who PND and PGT for HBOC considered to be acceptable. A white bar shows the answer from the clinical geneticists who PND and PGT for HBOC considered to be neither. A grey bar shows the answer from the clinical geneticists who PND and PGT for HBOC considered to be unacceptable.
The primary reasons to answer PND for HBOC to be “acceptable” were “1) to respect the client’s Autonomy” (93.3%, 14/15). Other reasons included “4) because there is a possibility that treatment and prevention for HBOC reduce QOL and body image” (33.3%, 5/15), “9) because it’s OK if the criteria for implementation are met” (33.3%, 5/15). The reasons to answer PND for HBOC to be unacceptable include “2) because HBOC is an adult-onset disease” (72.7%, 32/44), “3) because HBOC is “actionable” disease” (63.6%, 28/44), “7) because the penetration rate is not 100%” (56.8%, 25/44), “8) because PND is a test that considers abortion of pregnancy” (43.2%, 19/44). The reasons failed to choose either acceptable or unacceptable about PND for HBOC were “2) because HBOC is an adult-onset disease” (55.6%, 15/27), “1) To respect the client's Autonomy” (48.1%, 13/27), “3) because HBOC is “actionable” disease” (40.7%, 11/27), and so on.
The reason to answer PGT for HBOC to be “acceptable” was also “1) to respect the client's Autonomy” (85.7%, 24/28). The reasons to answer PGT for HBOC to be “unacceptable” include “2) because HBOC is an adult-onset disease” (58.3%, 21/36), “7) because the penetration rate is not 100%” (44.4%, 16/36), “6) because there is a wide range of phenotypes” (38.9%, 14/36). The reasons in the clinical geneticists failed to choose either acceptable or unacceptable about PGT for HBOC” were “2) because HBOC is an adult-onset disease” (40.9%, 9/22), “1) to respect the client's Autonomy” (36.4%, 8/22), “11) because there is no legal system for genetic discrimination in Japan” (36.4%, 8/22).
In contrast, there were no marked differences in the reasons provided for stated attitudes toward PGT for HBOC between healthy individuals and cancer patients. The following comments were made by respondents who considered PGT to be acceptable: “We have the right to know and it’s good to have more options for reproduction”; “PGT is a good way for avoiding future disease risks for the children”; “Some people will not carry out PGT even if they can choose it, so it is good to be provided the freedom of choice”; “Because the subject of the testing is not a fetus but a fertilized egg, it feels less resistance to choice”; “It’s good to have PGT for those who want to have a ‘genetically’ healthy child.” A woman who had received assisted reproductive technology (ART) stated, “I had difficult experiences in IVF (in vitro fertilization) treatment and I think it is better to be able to choose a fertilized egg to implant.”
On the other hand, respondents who considered PGT to be unacceptable commented: “PGT for all disorders and diseases will lead to choose the person who should not be born”; “Only the chosen one will be born”; “Everyone has some faults such as a disease”; “Even if PGT is implemented for specific diseases, the possibility of developing another disease cannot be eliminated.”
We conducted a survey to understand attitudes toward PGT for HBOC in Japan and found the striking difference among the members of the lay public, including healthy people without history of cancer and breast/ovarian cancer patients, and the clinical genetic professionals. In short, more than half of the laypeople (55.1-61.9%) considered PGT for HBOC to be acceptable, but only 30.9% of the genetic professionals considered it to be acceptable (Table 2). In the healthy and patient groups there was no significant difference in the proportion of respondents who considered PND and PGT for HBOC to be acceptable, but in the genetic professionals more respondents considered PGT for HBOC to be acceptable than those who considered PND to be acceptable. The most frequent chosen reason that PND and PGT for HBOC considered to be acceptable was the client's Autonomy and the most frequent chosen reasons that PND and PGT for HBOC considered to be unacceptable were things related to disease characteristics of HBOC such as its adult-onset, incomplete penetration and actionability that is the availability of preventive and therapeutic options.
High acceptability of PGT for HBOC in the oversea made it possible for the academic societies to approved. The European Society of Human Reproduction and Embryology (ESHRE) ethics taskforce argued that PGT was acceptable for adult onset and multifactorial diseases in 2003 [6]. In the United Kingdom, the Human Fertilisation and Embryology Authority (HFEA) extended licensing of PGT to include genetic susceptibility to incompletely penetrant, adult onset hereditary cancer, including HBOC, in 2006. The HFEA’s Ethics and Law Committee recommended that: “Conditions where the quality of life is severely affected or the length of life is shortened would be considered to be severe” and reasoned that breast, ovarian and HNPCC cancers are “serious genetic conditions because they cause suffering and are life-threatening,” and that therefore “PGD should be available to test for these cancers” [9]. PGT is considered more acceptable and advantageous because it would prevent transmission to future generations7. In the Netherlands, PGT was introduced in 1995 and, after nationwide political and ethical discussions, approved for late onset inherited cancer predisposition syndromes in 2008. Nowadays, HBOC is one of the most frequent indications for PGT [8]. In the U.S.A, PGT is one of the options for people who carry a gene mutation of hereditary cancer syndrome and desire having a child [10].
An overseas meta-analysis reviewed 13 studies on PGT acceptability and showed that the acceptability of PGT to other high-risk people was relatively high (71%) [11]. Compared this survey data to the meta-analysis data, it was found that the acceptability of PGT for HBOC was likely to be lower in the Japanese breast/ovarian cancer patients. In other hands this survey was revealed that over 30% of the genetic professionals had the experience of being asked about PND or PGT for HBOC from their clients in genetic counseling. This fact showed that a certain extent number of BRCA1/2 mutation carriers considered PND or PGD as a reproductive option. Currently in Japan, PGT and PND cannot be applied to HBOC under the requirements. In Japan the “serious” hereditary diseases are limited to childhood-onset disorders, but the definition of severity or seriousness may vary depending on the beliefs of the patients, their families, and the genetic professionals individually. Therefore, in Japan as well, it may be necessary to discuss the definition of severity or seriousness from the perspective of "Quality of Life through one’s whole life." In addition, surveys of attitudes toward PGT for HBOC among Japanese BRCA1/2 mutation carriers is needed and support systems to aid reproductive decision making for younger couples without options of the reproductive genetic testing should be discussed [7].
In Japan, PGT-M is adopted just for childhood-onset severe disorders and not for late-onset disorders such as HBOC. Although the age of onset is a major element in the evaluation criteria for disease severity, the adequate cut-off age in each couple or each affected person is unclear. it may be necessary to discuss the definition of severity or seriousness from the perspective of Quality of Life through one’s whole life. In the settings of genetic counseling the way of the psychosocial support system for the couples with a BRCA1/2 mutation should be discussed.
Limitation of This Study
The response rates of the questionnaire were 25.1% in the certified genetic counselors and 29.4% in the clinical geneticists. Therefore, the answers in the genetic professionals were limited and further data collection is needed to generalize. However, the data from the over one hundred genetic professionals who have been providing genetic counseling related to HBOC is very valuable. In addition, this report did not include the subjects who have a BRCA1/2 mutation. The survey for the parties (BRCA1/2 mutation carriers) concerned this issue must be conducted immediately.
This research was supported by JSPS KAKENHI Grant number JP 17K17689 and 20K18159.
The authors declare that they have no conflict of interest.
The datasets generated during the current study are available from the corresponding author on reasonable request. The data are not publicly available due to privacy or ethical restrictions.
- Fortuny D., Balmaña J., Graña B., Torres A., Ramón y Cajal T., et al. (2009) Opinion about reproductive decision making among individuals undergoing BRCA1/2 genetic testing in a multicentre Spanish cohort. Hum. Reprod 24: 1000-1006. [Crossref]
- Chan JL., Johnson LNC., Sammel MD., DiGiovanni L., Voong C., et al. (2017) Reproductive Decision-Making in Women with BRCA1/2 Mutations. J. Genet. Couns 26: 594-603. [Crossref]
- Terui-Kohbata H., Egawa M., Yura K., Yoshida M (2020) Knowledge and attitude of hereditary breast cancer among Japanese university female students. J. Hum. Genet 65: 591-599.
- Sandelowski M., Barroso J (2005) The travesty of choosing after positive prenatal diagnosis. J. Obstet. Gynecol. Neonatal Nurs 34: 307-318. [Crossref]
- Wagner TMU., Ahner R (1998) Prenatal testing for late-onset diseases such as mutations in the breast cancer gene 1 (BRCA1). Just a choice or a step in the wrong direction? Hum. Reprod 13: 1125-1126. [Crossref]
- Shenfield F., Pennings G., Devroey P., Sureau C., Tarlatzis B., et al (2003) Taskforce 5: Preimplantation genetic diagnosis. Hum. Reprod 18: 649-651. [Crossref]
- Ormondroyd E., Donnelly L., Moynihan C., Savona C., Bancroft E., et al. (2012) Attitudes to reproductive genetic testing in women who had a positive BRCA test before having children: A qualitative analysis. Eur. J. Hum. Genet 20: 4-10. [Crossref]
- Derks-Smeets IAP., Gietel-Habets JJG., Tibben A., Tjan-Heijnen VCG., Meijer-Hoogeveen M., et al. (2014) Decision-making on preimplantation genetic diagnosis and prenatal diagnosis: a challenge for couples with hereditary breast and ovarian cancer. Hum. Reprod 29: 1103-1112. [Crossref]
- Krahn T (2009) Preimplantation genetic diagnosis: does age of onset matter (anymore)? Med. Heal. Care Philos 12: 187-202. [Crossref]
- Donnelly LS., Watson M., Moynihan C., Bancroft E., Evans DGR., et al. (2013) Reproductive decision-making in young female carriers of a BRCA mutation. Hum. Reprod 28: 1006-1012. [Crossref]
- Quinn GP., Pal T., Murphy D., Vadaparampil ST., Kumar A (2012) High-risk consumers’ perceptions of preimplantation genetic diagnosis for hereditary cancers: A systematic review and meta-analysis. Genet. Med 14: 191-200. [Crossref]