Introduction: During embryology of the nasal cavity, posterior choana forms by canalization or obliteration of the fold between olfactory groove and roof of the primitive oral cavity. A failure of canalization of this aperture is referred to as choanal atresia.
Case Summary: A 10-day old female neonate was admitted into the out-born section of our special care baby unit (SCBU) via the children emergency ward (CHEW) on account of nasal obstruction and difficulty to breath which was noticed immediately after birth. A diagnosis of bilateral mixed (bony and membranous) choanal atresia was made and child subsequently had bilateral choanoplasty. Nasal stents remained insitu for 3 months from the day of operation, after which stents were finally removed.
Conclusion: Diagnosis of Choanal atresia should be preceded by a high index of suspicion following clinical presentation of respiratory difficulty which improves with crying in a new-born baby and inability to suction through the nasal cavities following birth. In the absence of conventional instruments for choanoplasty, an improvised metallic probe can be used to canalise the posterior choana.
Recommendation: We advocate that stent stays for at least 12 weeks before removal to ensure long lasting patency of posterior choana.
The nasal aperture also known as the posterior choana is the opening at the posterior end of nasal cavity through which air flows from nose to the nasopharynx. During embryology of nasal cavity, posterior choana forms by the canalization or obliteration of the fold between olfactory groove and roof of the primitive oral cavity. A failure of canalization of this aperture is referred to as choanal atresia [1]. It is an anatomical abnormality which can be unilateral or bilateral depending on the side of the nasal cavity involved. It is a rare abnormality occurring in 1:7000-8000 births, and a notable cause of congenital nasal airway obstruction [2]. Choanal atresia is said to be commoner in females than males, and can be classified as bony, membranous or mixed. However, as much as epidemiology of 90% bony and 10% membranous has been described, purely membranous type of choanal atresia is rare because it can easily be perforated during immediate post-natal suctioning in new-born, and thus not observed or reported [3]. Most cases of Choanal are seen in isolation, but it has been considered to be in association of other malformations. These associated congenital abnormalities occurring with choanal atresia include Coloboma, Heart disease, choanal Atresia, Retarded growth, Genital hypoplasia, and Ear anomalies, which are collectively referred to as CHARGE syndrome [4].
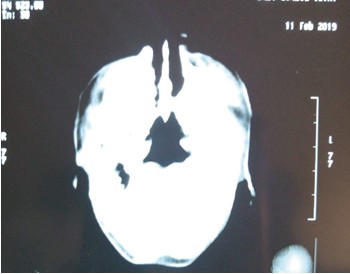
A 10-day old female neonate was admitted into the out-born section of our special care baby unit (SCBU) via the children emergency ward (CHEW) on account of nasal obstruction and difficulty to breath which was noticed immediately after birth. She was referred from a peripheral hospital where she had been delivered preterm at a gestational age (GA) of 34 weeks and 5 days. The birth weight was 2.3kg, with an Apgar score of 5 and 7 at 1 and 5 minutes respectively. Pregnancy was supervised at the referring centre, from the 16th week of gestation. Mother attended regular antenatal visits at the peripheral centre where child was born and was taking her routine ante-natal drugs regularly. During antenatal visits, Pregnancy was monitored and serial ultrasound scan done showed placenta previa, with otherwise normal findings. However, pregnancy was complicated by drainage of liquor at 20-week gestational age, which was managed conservatively. There was no history of maternal febrile illness or rash, in this pregnancy, and it was carried to 34 weeks GA, when mother developed bleeding per vagina with uterine contractions. She had emergency caesarean section for placenta previa at 34 weeks and 5 days gestational age. Following delivery, the nurse attending to baby observed severe chest in-drawing on breathing, with cyanosis. An attempt to pass a naso-gastric tube for suctioning of nose was met with stiff resistance. At presentation in Children emergency ward, physical examination showed that baby was cyanotic, in respiratory distress with substernal and subcoastal recession, all of which improves with crying. Baby’s condition improved with an oropharyngeal airway placed in situ. She was not pale, was afebrile with a temperature of 36.8oC, and oxygen saturation was 98% on room air, with bilateral nasal discharge. On central nervous system examination, anterior fontanelle was flat and normoactive, the occipito- frontal circumference was 32cm, suck and grasp reflexes were good, and the general muscle tone was normal. On respiratory system examination, respiratory rate was 48 cycles per minute, with vesicular breath sounds with occasional transmitted breath sounds. On cardiovascular system examination, heart rate was 130 beats per minutes, and only heart sounds 1 and 2 was heard. On abdominal examination, her abdomen was full, moved with respiration, soft, and no organomegaly of the liver, spleen or kidney. Genito-urinary system examination showed matured female external genitalia and anus was also patent. Physical examination revealed no other congenital abnormality. An oro-gastric tube was placed insitu for feeding since child was unable to breastfeed. At this point, a computed tomography scan of the nasal cavity was done, which reported narrowing of the posterior choana, right measures 0.59mm and left 1.17mm (normal range being 3mm. Thickening of posterior vomer measuring 5.9mm (<5mm), membranous closure of the nares was also shown (see figure 1).
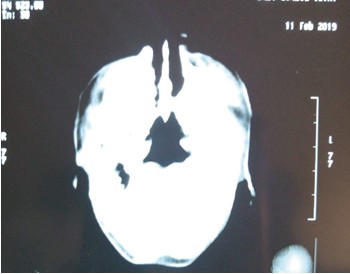
Figure 1. Computed Tomography Scan of Patient Showing Bilateral Bony Choanal Atresia
A diagnosis of bilateral mixed (bony and membranous) choanal atresia was made, and the child was booked for emergency bilateral choanoplasty. Pre-operative blood tests showed packed cell volume of 38%, balanced electrolytes and no sign of infection.
The child subsequently had bilateral choanoplasty under general anaesthesia. Intra-operatively, with patient lying in supine position, general anaesthesia was given, and orotracheal tube of appropriate size was inserted. Child was then put in Rose position, neck extended with roll under shoulder, and head stabilized on a head ring. Blair’s head draping, and general body draping was applied. Mouth was opened using a Boyle Davis mouth gag, suspended on a bipod stand, and stabilized on a Magruarian plate. Pharyngeal secretions suctioned, and pharynx packed. After nasal cavity was suctioned, bilateral bony atresia was confirmed, with membrane covering the anterior aspect of the bony plates. A solid metallic probe was introduced into the right nasal cavity, up to the atretic plate covering the posterior choana. Firm pressure was applied to probe, and right posterior choanal perforated. Similar procedure was repeated on the left side, to perforate left posterior choana. Choanal openings were then widened with serial insertion of increasing size of feeding tube. Nasal stent (improvised with 5cm length of nasogastric tube size 10), was applied in both nostrils as one continuous tube (with fenestrations behind the nasal bone and the choana) and secured over the columella (see figure 2).

Figure 2. Picture Showing Child Immediate Post-Op, with Oropharyngeal Airway, Nasal Stents, and Nasogastric Tube in Situ
Nasogastric feeding tube and oropharyngeal airway was placed insitu, Pharyngeal pack was removed, and patient reversed by the anaesthetist. Estimated blood loss was about 5-10mls, and procedure was well tolerated by patient. Patient was taken to recovery, before returning to SCBU.
Post-operatively, oropharyngeal airway and feeding tube remained for 24 hours before removal, and secretions in nasal cavity and stent were suctioned on a PRN basis. Physical examination during the post-operative period showed a conscious baby, no sign of respiratory distress, acyanosed, afebrile (37oC), with normal systemic examinations. Baby’s weight and feeding was closely monitored, and both progressively improved over the next couple of weeks, as well as nasal secretion, which had reduced in quantity. Mother was taught how to suction child’s nasal cavity and stent at home, using a size 6 suction tube which has been cut to half its length, attached to a 10 ml syringe. Child was discharged home on the 14th post-operative day, during which she had made marked improvement. Her weight on discharge was 2.5kg, and she was discharged home on oral antibiotics, decongestant, and nasal saline spray for irrigation and loosening of crusts, with an instruction given to mother to suction child’s nasal cavity and stent PRN.
On follow up, visit 2 weeks after discharge, child’s breastfeeding and breathing have improved, and her weight had increased to 3.0kg (see figure 3).

Figure 3. Picture of Child at 2 Weeks Follow Up Visit
A) Child is Seen Sleeping Calmly with Mouth Closed, No Cyanosis, and No Respiratory Difficulty
B) Child is seen during Breastfeeding, No Difficulty in Breathing, No Cyanosis. (White Arrows Showing Nasal Stent in Situ).
*Photos with due permissions obtained.
Nasal cavities were dry, but mother admits to occasional removal of crusts from child’s nasal cavities. Nasal stents remained insitu for 3 months from the day of operation, after which stents were finally removed and after a follow up of 8 months; there was neither complication nor re-emergence of cyanotic spells and respiratory symptoms.
The index case was suspected to be choanal atresia immediately after birth; however the process of referral, diagnosis and treatment was responsible for the delay, such that the substantive surgical treatment was carried out 10th day after delivery. There are various factors responsible for this delay, such as unsteady power supply to carry out requested investigations in hospital, low financial power of parents of the baby who have to paying out of pocket for these hospital investigations, theatre fee and treatment requirements. In addition is shortage of manpower in the hospital, leading to a line-up of emergency cases on the waiting list of the anaesthetic emergency team on call, leading to prioritization of emergency cases. However, the time interval between delivery and definitive treatment in our case is still considerable, in the case series reported by Manica et al,[5] duration between birth and definitive treatment ranged from 1 day to 2 months [5]. The authors however did not give likely reason for the delay in the cases reported.
The diagnosis of this condition is usually facilitated with computed tomography scan [6]. This was the case in this patient, where CT scan showed features of bony atresia which are in keeping with the report by Slovis et al. [6] with medial bowing and thickening of the lateral walls of the nasal cavity with enlargement of the vomers, which may be fused to the lateral wall of nasal cavity. In membranous atresia, lateral wall of nasal cavity is minimally affected, and the vomer usually appear normal [6].
Opening of the bony atresia was done using a metallic eustachian tube canula as an improvised perforator; however, serial dilatation was done by passing successively increased size of feeding tube through both posterior choana. Manica et al in their study similarly improvised with the use of metallic suction tube, however, after opening, they widened the choana using a microdebrider under endoscopic vision [5]. After serial dilatation of the choana, feeding tube size 10 was left insitu as stent. It was passed through both choana as a continuous tube with both ends emanating at both external nares respectively and anchored across the columella. This is contrary to some studies where endotracheal tube was used as the stent [3, 5].
The stent in our patient was left for 12 weeks, and after a follow up of 8 months, there was neither complication nor re-emergence of cyanotic spells and respiratory symptoms. This was also the case in the studies by Gupta and Kour in 2017 [3] and Manica et al in 2014, [5] where no complication was noted. However, the study by Abdullah et al in 2012 reported a case of bilateral choanal atresia where the removal of the stent 6 weeks after choanoplasty was followed by resurgence of cyanotic spell in the child [7]. They further stated that a repeat choanoplasty had to be carried out a week later and stent left in place for a longer time. This indicates that following choanoplasty, the longer the stent stays the more unlikely for the choana to block, and the more unlikely cyanotic spells will return.
The diagnosis of Choanal atresia should always be preceded by a high index of suspicion following clinical presentation of respiratory difficulty which improves with crying in a new-born baby and inability to suction through the nasal cavities following birth. In the absence of conventional instruments for choanoplasty, an improvised metallic probe can be used to canalise the posterior choana. We advocate that stent stays for at least 12 weeks before removal to ensure long lasting patency of posterior choana.
- Ganesh E, Siva BJ (2016) “Choanal Atresia” Embryological basis and its clinical significance. Elixir Embryology 100: 43719-43722. [Crossref]
- Goyal P, Kumar A, Goyal B (2014) Choanal Atresia. International Journal of Medical Sciences, Research and Practice 1: 61-62. [Crossref]
- Gupta M, Kour C (2017) Congenital bilateral choanal atresia: A rare case. J Rare Disord Diagn Ther 3: 1-4. [Crossref]
- Saleem AF, Ariff S, Aslam N, et al. (2010) Congenital bilateral Choanal Atresia. J Pak Med Assoc 60: 865-872. [Crossref]
- Manica D, Schweiger C, Saleh Netto CC, et al. (2014) Retrospective study of series of Choanal Atresia Patients. Int Arch Otorhinolaryngol 18: 2-5. [Crossref]
- Slovis TL, Renfro B, Watts FB, et al. (1985) Choanal Atresia: Precise CT evaluation. Radiology 155. [Crossref]
- Abdullahi AB, AbdulRahman RB, Aziz SB, et al. (2013) Management of congenital choanal atresia (CCA) after multiple failures: A case report. Med J Maylasia 68: 76-78. [Crossref]