This inhuman disease has still today no medication that can cure it. We can with a good movement program give a contribution to the quality of life for this group of patients.
As a physical therapist, we often stand on the “side-line”, but that isn’t the place where we belong, we have the skills and knowledge about older people and their needs, therefore must this group have also our greatest interest and treatment possibilities.
In the last 20 years that we give courses and have treated so many people with this devastated disease, we have developed a way of working that can help in slowing down this disease but for all can give these people a way of life that focus on a degree of independence, so long as possible.
But that asked above all, for a good team and the willingness of us, to make part of that team.
That asked also that we observe the environment in which people live and move and see what obstacles we create and how we can change that and make the independency possible.
We have often deal with older and frailty, people but it is also a neurological disease.
A disease that damaged the brain and not only in the higher cognitive functions and memory etc. but also has this brain damage influence on the mobility and the motoric.
This must be assessing to get a good treatment program and to do that treatment program, you must understand what the mental possibilities are of this people to get a connection and make a treatment work.
Still it is a degenerative disease, this asked therefore also for the knowledge what is possible and what not anymore. Because this patients will give you a total other behaviour when they are “over-asked”!!
This asked more from everyone working with patient with dementia, not only knowledge about the motoric of the elderly, but also about neurological diseases and, above that, the skills to create a climate in which this patient can exercises with pleasure.
Dementia; Rakt Scheme; Capacity
Writing a series of articles about the physical treatment of people with dementia isn’t possible when there is no multidisciplinary approach in which the physical therapist is part of.
Only exercising with no translate to the everyday reality, will be a treatment that isn’t coping with the problems that this people experience every day.
The surrounding in which people live must be changed to get the best enriched environment [1] in which movement is stimulating but also give the support that is necessary.
To convince people, all people family, nurses, staff etc. of the importance of movement to counter this terrible disease, must this treatment be realistic because we dealing with an group people that getting older and through the disease their possibilities will decrease and nobody-Nobody-can perform the whole day on his maximum level.
That asked for a good assessment that is often possible at the beginning of the disease and give us the tools and insight what is less and what can be changed. That means that exercising in the beginning is possible and that through the stimulating of the blood-brain system [2, 3, 4, 5]. The disease can slowing down but when the disease progress than will independent moving be a top-action. There will be a moment that aids are needed but what aid we want and which aid we want not and why not.
Remarkable is that the most people no signs of dementia give as an important complains by the local doctor that the walking and balance is worse [6]. This isn’t counting for all different types of dementia but what we taught that memory was the first sign or cognitive lesser function, was their investigation: “That 5 year before the diagnosis was done that this people visited the local doctor often with walk complains”. They were often than others of equal age by the doctor and their complains were pointed on walking etc.
It is still today the question when we must start with the treatment. We think that an good moment is when people need an walking aid and especially an rollator frame, because this an sign that the balance isn’t good anymore and this rollator frame will increase some independency but also change the balance performance and not always in an good way.
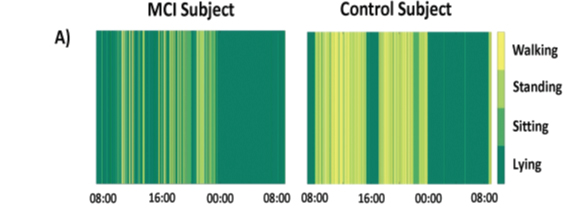
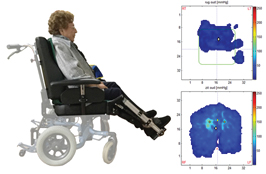
This hasn’t be investigated but in our own investigation, we had the possibility to see what happens with 5 older people with an diagnosis M.C.I.- (Mild Cognitive Impairment) and the use of an rollator frame. That the quantity and quality of the movement by this group is changing is already investigated and was very clear, see figure 1 [7]
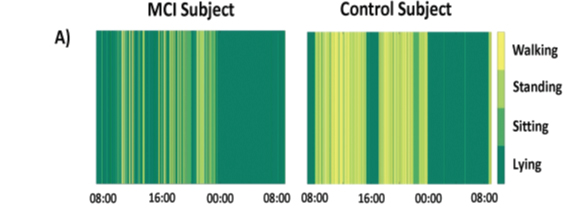
Figure 1.
The green colour through the day! [7]. is colour lighter than there is a lot of activity but when the colour is darker is little movement. What we observe is that the group with M.C.I. has much more darker green through the day what is associated with lying and sitting. This gives an indication that this group move much lesser. But our job must be, to investigate why this is happen!!
Table 1. Gives an Indication What Happen with 5 Patients with M.C.I That Receive a Rollator Frame to Walk More. We Did a Balance Check
Patients |
After one month |
After two month |
After three month |
1. Mister B. > 30sec |
25 sec |
20 sec |
18 sec after 3 trials, best performance |
2.Madame C. >30sec + |
20 sec with eyes closed |
20 with but without eyes closed |
19 sec |
3. Madame O. >30 sec |
20 sec. |
15 sec. |
15 sec |
4. Mister I. > 30sec + |
25 sec with eyes closed |
20 sec with the eyes closed |
15 sec with eyes open |
5. Madame R.>30sec+? |
18 sec |
14 sec |
10 sec |
These 5 persons walk the whole day with the rollator frame also on several places in their home and there was an amount of support on it. At the start where the all 5 capable to do a one leg standing-test [8] score above the 30 second and patient 2 and 4 could this with the eye closed. Patient 5 say that he has also his eyes closed but we don’t believe him. With the rollator frame they walk more and also greater distance and that has a good effect on the aerobe possibilities but the balance was reducing fast, too fast. To slow this loss, we started a balance training program.
This loss of balance was a perceptual change, especially lateral:
The people were not able to shift the hip over the foot; there was after one month a movement of the upper trunk [9, 10] instead of a lower trunk shift. The power of the muscles around the hip especially the abductors was enough after one month but starting after two month to decrease and this was worse after three months and need exercising. But the first item-a wrong perceptual scheme-was the first sign and this is very important, because this effect can be the reason that the power of the abductor are so fast decreasing. People with dementia have a decreasing body scheme perception (Kraft and others), that has a direct relation with this disease.
Furthermore we know that the tone by these group patients can change. This Paratonia [12, 13] can occur in the beginning of this disease and tone increase means more pathological synergy [14, 15, 16, 17, 18, 19] and therefore an loss of selectivity that makes balance control and correction much more difficult. But we know also that more tone goes hand in hand with less perception and loss of projection in the cortex [20, 21, 22, 23, 24, 25].
In this series of articles about quality of life for people with dementia from a physical therapist point of view, there are different points that must be spoken off to get a complete picture.
This is impossible within one article therefore we make 6 chapters to get a complete picture with information at the right moment in the process of the disease.
A. Chapter one will describe what the sciences have found to slow the process of dementia, and an attempts to translate this to the reality.
This with the introduction of the “Rakt-concept”, an concept that try to get the possibilities of the patient with dementia in the divers stages of the disease in the picture and try to warn for too “much” because the brain system by this people is less tolerable and will react with primitive reactions = “run or hide “.
B. Chapter two will handle over the assessment in the earliest stadium as possible and how to get so long as possible information what is happen in brain and body of the patient.
C. Chapter three will focus on people that walk at home or in a long care setting and how we can stimulate an training. Balance wills here have a central place. In the Rakt-concept is this phase 4.
D. Chapter four will focus on people, that have problems to move on their own in, in and out bed, in and out a chair /toilet/douche etc. and walking. In the Rakt-concept is this phase 3.
E. Chapter five will focus on the group that is depend of an wheelchair and which wheelchair is the best solution for every individual and how we can use the remaining functioning to move and avoid aids that make things worse. In the Rakt-concept is this phase 2.
F. Chapter six will focus on the last stage of this disease; the foetal (fetal) attitude and what possibilities we have than to get some influence on the quality of life. The focus lies on the abnormal high tone that an group of this patient develop. In the Rakt-concept is this phase 1.
“Normal” motoric of elderly: That isn’t right, because there is no normal motoric of older people but this is an adaptation of older people on all kind of decreasing functions and that gives a picture that is important to discover and asked an individual assessment. Learning or “re-learning” is thinking, [27] where we can set a lot of question marks. Let’s look what can cause the balance problematic.
The problem in the beginning of the disease is on physical area also always the balance. We-therapist- are train this people to restore the balance possibilities and call it “fall-prevention “. We try to teach the patient to adapt on the problems and search for a solution that this can prevent the danger of falling. But [27, 28, 29] often is the border of the adaptation all there and that means that further adaptation isn’t possible or we search for hidden failures. In the investigation mentioned before [27] is power investigated that older healthy adult had in the dorsal and plantair flexoren. This was (table 2) significant lower than healthy young people and that loss of muscle power is an reason that an good physical treatment can give an result what give the adaptation some air for some time [27].
Table 2
Strength difference |
Healthy young people |
Healthy elderly |
Re dorsal flexors |
11.7 Nm/Kg |
8.2 Nm/Kg |
Li dorsal flexors |
11.6 Nm/Kg |
8.6 Nm/Kg |
Re plantar flexors |
19.2 Nm/Kg |
11.3 Nm/Kg |
Li plantar flexors |
21.7 Nm/Kg |
12.2 Nm/Kg |
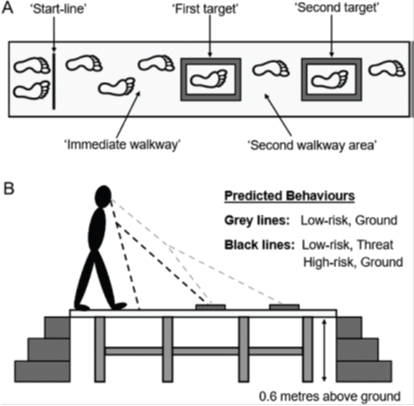
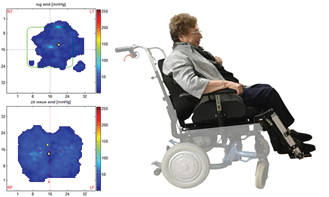
Elderly use an alternative system. Elderly walk slower and use the eyes not as scanner from the environment but for scanning and control of the environment in direct front of them and their feet/body. How that scanning works see we in this investigation:
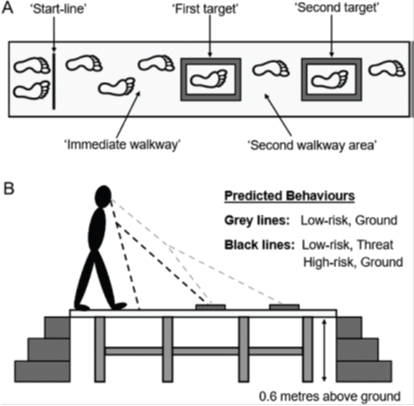
Figure 2.
Walking on a platform a meter above the ground and avoid obstacles. The elderly adapt their speed but also look directly in front of their feet. Not all but the most make this adaptation and the young ones have their eyes pointed on the obstacles. That makes an adaptation on speed not necessary and they can do the walking with greater speed and less mistakes [30].
“Learning “to look further to front is a mistake because this brain has develop a solution within their possibilities!
What Teach Science Us?
In the book about the progress in healing of the disease Dementia [2] was the conclusion that no medicament has found, that was able to slowing down this disease and certainly was healing no option. Still there was a remark that the amount of people that would have in future this disease was lower than the expectation from 10 years before.
The reason for this decreasing numbers was the better care for hart diseases that has also an effect on the blood circulation in the brain and that was an sign that investigator search for an increasing of this blood circulation to get better result.
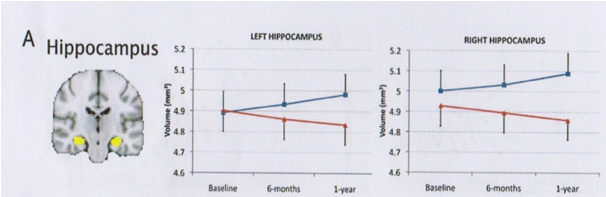
One of them was Prof. Erickson [31] who investigated the size of the hippocampus through an M.R.I. image. He takes M.R.I. image at the beginning of the investigation after 6 months and after a one year.
He divided at random his elderly without dementia in two groups:
One group (blue line) get walking training ones an week, starting with 5 minutes and increasing to a level of 40 minutes. The first week was the heart rate 50-60% of the maximum after that was it increased to 60-75%. That means that there was training with an intensity of almost 75% of the maximum heart rate one week for 40 minutes.
This is Aerobe Training with a Progressive Intensity Load!!
The other group (red line) receive ones a week stretch and strengthening exercises with an increasing load.
This is anaerobe training with increasing load, but not task specific.
The result see figure 3.
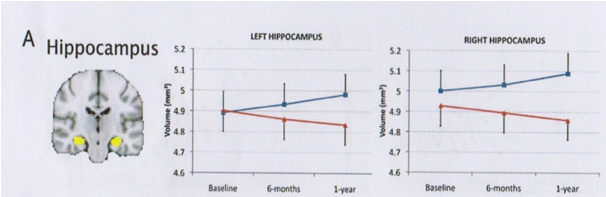
Figure 3.
Image by M.R.I reveal that the blue line group had an increase of the hippocampus (right and left) of 2%.
The red line group had the normal decrease of 1-2 %.
That means that elderly when they exercise aerobe with a certain intensity were able in the beginning the decrease of the hippocampus to brace and even to change it in a progression of 2%. That means that the vulnerability of the hippocampus is decrease and that is a sign that the disease could be postponed.
This type of investigation is done more and almost always was there a clear sign:
Intensive aerobe training gives a better functioning brain through a better blood circulation and also through that circulation and lesser inflammation activity in the brain but there were also sign that not all people response on the same way. The intensity of the heart rate was a clear load, but not everyone respond. There was a group of responders and non-responders. When it was possible than was the combination aerobe with cognitive demands the best option. [32, 33, 34, 35, 36]. This will increase the possibilities but for not everyone, but on bicycle for an television is an option that many older people can do and we can than achieve an aerobe training with an double tasking on the television.
But is this also the Possible by People that has this Disease?
In the beginning (Rakt-concept phase 4) is this possible but this will be very difficult in the later stages and remarkable the later stages are less frequent in the picture by the scientists.
About the aerobe training we have investigation that this confirms. Dr. Bossers give this conclusion after his investigation in 2015, quote: “Compared with a non- exercise control group, a combination of aerobic and strength training is more effective than aerobic-only training in slowing cognitive and motor decline in patients with dementia. No mediating effects between improvements in cognitive
Function via improved motor function was found”.
He has it over a combined treatment with an aerobe element but there was also the discussion what must be the intensity and is that equal for everyone. And an extra aspect was: Not everyone is a mover, what must be them the approach?
The reaction on the cognitive levels is by this group of patient in the beginning of their dementia small but significant and gives therefore the positive assumption that this can slow done the disease.
When we see by people with dementia what is fast a problem than is that the ADL (All Day Living) activities than his next investigation in 2016 was positive with a light nuance.
Quote: “Physical exercise can improve ADL levels in individuals with dementia, but improvements are small and seem independent of exercise type. Additional analyses suggest that combined aerobic and strength exercise may be more effective than aerobic-only exercise to effectively target ADL dysfunction in individuals with dementia”.
But there is a positive result and the ADL possibilities are high brain function with a lot of cognition as describe by lot of investigators. [39, 40, 41, 42].
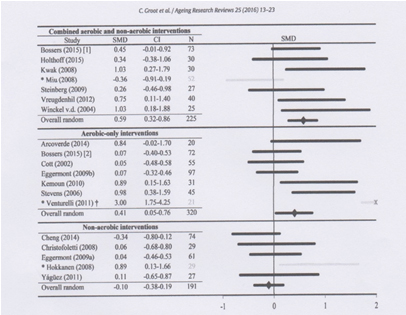
But in both investigations there is not only an aerobe approach but also a strengthening program. The meta- analyses, that has perform by this group investigators gave the following outcome:
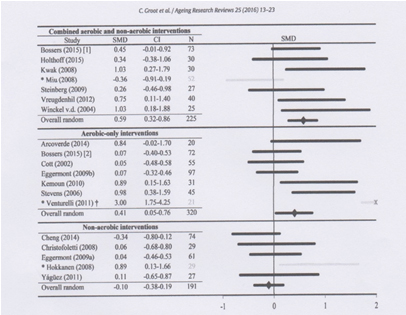
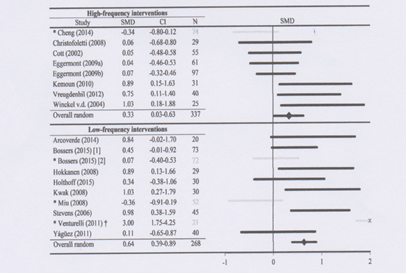
Figure 4.
Combined aerobic and non-aerobic intervention give in all articles the best results on the cognition of the involve patients. The aerobic invention with the intensity as describe by Erickson has also a positive effect on the cognition. Non-aerobic invention and that were mostly strengthening exercises or stretching has no effect on the cognition.
Often is the greatest problem with these investigations that the form of the exercises isn’t described and the reliability is than very poor. Here must the science be clear and use the TIDieR (Template for Intervention Description and Replication [44]) scale to get this for everyone understandable.
When we give a strengthening exercise with a leg press-par example-than have we a muscle strengthening that isn’t task specific and will have a long transfer to the function and the benefit for the patient will be less and less fast and has this aerobe effect on the right level.
This meta-analysis also found that frequency of therapy wasn’t so important. The bottommost frequency of two times a week scored higher than the therapy with a higher frequency.
We know now something about the intensity for the aerobe part but very little about the intensity of the non-aerobic part.
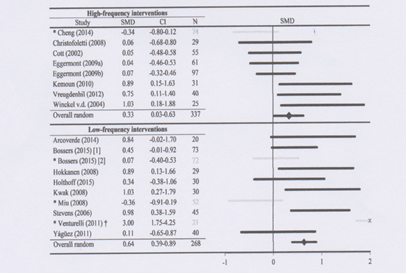
Figure 5.
The frequency of the interventions and their effects. Upper part the group with highest frequencies of the interventions and the effect on the cognition. The lower part with the lower frequency. Twice a week as bottom and that is more than most nursing homes can offer their patients.
We know that exercising has an positive effect on cognition also by people with dementia, There must be an aerobe component be present that must give an heart rate increase of approximately 60%. We know also that anaerobe is important but with which intensity isn’t clear.
By all therapy of neurological diseases the best approach is task specific [45] and that count also for balance, walking and IADL and ADL training. Important is that we have a reference what the normal performance is from elderly at a certain age.
To fast is a rollator frame and normal think by elderly and isn’t there no question, why this rollator frame is so important and why walking and standing without isn’t possible anymore. This was obvious when in our Nursing Home a daily-caring ward was open. The question wasn’t what physic problems there where. The burden of the people at home was the indication to get this group to a daily caring ward.
Of the 35 people 33 walk with a rollator frame and 2 with a stick and all had a BBS (Berg Balance Scale) [46] lesser than 45 and had therefore balance problems.
Also the T.C.T. (Trunk Control Test) [47] wasn’t by 18 person 100 and that means that the people at home must give assistance or that there were aids on bed to make it possible that this person was able to get in and out bed. The movements in bed were low [48] as we know of Parkinson patients with H&Y [49] of 3 and more. Still there was no indication for a therapy.
To convince the doctor that there was an indication we use the Senior Fitness Test [50] of Rikli and Jones. They have done a great investigation with a great group of elderly and have all this person tested on 7 items and have the outcome placed in tables in which we now can see what someone of a certain age is expected to perform. This age categories are set by 5 years and start with 60 year and go till 94 and that different for man and women. Using these tables we were able to convince the medical staff that the entire day-care patient had a lower physic condition and power than their people of the same age.
And the remarkable result was after 3 months:
All the participants were better and of the 18 person with no TCT of 100 had now a good score only 2 had trouble with turning in bed. By 33 of the 38 was the BBS increase to a level of 50 till 56 only the two people that had trouble with the turning in bed had also a lesser balance performance and this two had also the most obvious tone increasing.
Of course will this level decrease, but now we were able to start on an optimal level.
Two tests were remarkable in their outcome and there was also a connection.
A score of lesser than 100 on the T.C.T. and a score of more than 15 seconds on the T.U.G. (Time Up and Go test) [51, 52, 53] was almost every time present and this was always walking with a rollator frame. This connection will be further analyzed in chapter 3 or 4.
The test items of the Senior Fitness test of Rikli and Jones were;
- 30- Second chair stand – In 30 sec stand and sit as fast as possible.
- Arm curl – in 30 sec bed the elbow with 2.27kg for women, 3.63 for men.
- 6- Minute walk- walking for 6 minute a counting the amount of meters.
- 2 minute step test- during two minute lift the knee above a certain point.
- Chair sit and reach- mobility test to reach the foot.
- Back scratch- to invest the mobility of the shoulder for the ADL.
Pain is by people with dementia an very important issue that must have our interest because we are able to see and feel of the joint , muscles etc. are “feeling “normal and we can by using pain scale for Dementia, to give an clear answer when people are not sure about the pain [54, 55]. Behavior problems but also discomfort in movement of wiliness to move has a direct relation with the pain that is expressed on another way or better, we don’t hear, that this people have pain.
They do it but on another way!!
Notice there face, breathing and behaviour, as mentioned in the pain scales.
Perception, Abnormal Tone and Sarcopenia
Two of these three elements that is common by elderly. But by people with dementia there is the abnormal muscle tone that gives us the connection with a neurological disease. Less perception and sarcopenia are more common but there are all lot signs that this is far worse by people with dementia and this asked for another approach through the physical therapist.
Par example and higher tone will decrease the speed of the movement but also will this make the diversity of movement difficult. People will move in a stereotype way [13-25].
And abnormal tone say something about the projection in the brain, and higher tone will be an answer of the damage brain than can only react on a lower level. That means that the perception of the body will be changed, decreased and especially the feet and the hand will “feel” lesser.
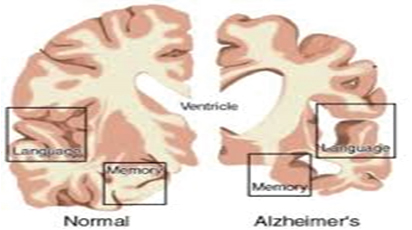
Figure 6
The difference between a cortex of a “normal “person and that of a patient with dementia. We see that the center for language and memory is damage but also the damage on the senso-motoric cortex. That means that selectivity is less and the tone/ and pathological synergy will increase.
Loss of the cortical structure will have consequences of good receiving and interpretation of the signals from the senses and will change the perceptual possibilities of this people. On the cortex lies great areas for the feet but the greatest are the hand and the month. The influence on the function of the foot/hand and month are therefore present often early as we see. That this is present in the beginning of this disease is not by everyone well-know, therefore do by everyone a tone investigation to be sure that this isn’t a reason why the function is decreased. This well investigated [12.13] and also by the disease of Parkinson [56] is this one of reason that balance impairment is so big. The loss of this cortical structures make that hand/foot and month are not capable so make fine and very much different movement and that cloudiness can be an sign that there is an loss of cortical structure. For the mouth can this give some problems with drinking and eating and swallowing and for the feet that they cannot react so fast and with great differently?
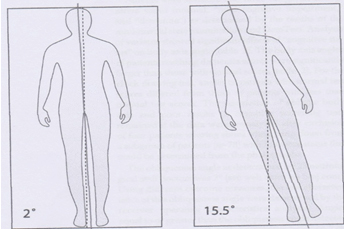
Very important is the discovery of Kraft and his colleagues [57] that by a cognitive impartment the total body perception is changing and that the total body axis is changing. We see such impairment by the severe stroke patient known as the pusher syndrome. This group has the “feeling that the middle axis of the body is more to the affected side as that is in reality.
Kraft say an oblique lying pattern till 15°,maybe the reason this people lie oblique in bed and are not well to correct. (Figure 6)
Figure 6.
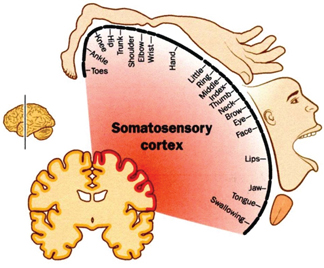
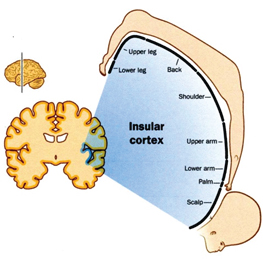
Figure 7 and 8, the normal somatosensory cortex with the huge projection of hand and the mouth and the center for speech and eating/swallowing process. When we look deeper in the brain than are there still projection but now are other structure more prominent and optimal performance of the hand and mouth need the somatosensory cortex (figure7).
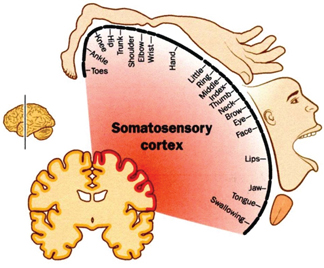
Figure 7.
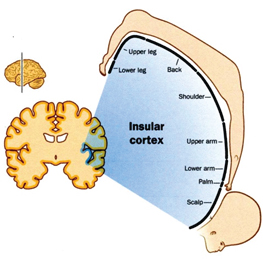
Figure 8.
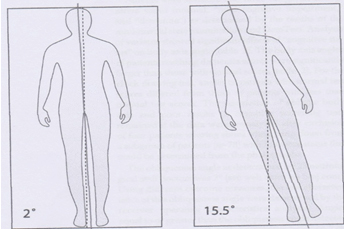
Figure 9.
The deviation that was found by people with a cognitive impairment and there chosen position in an lying position. This could be the reason why some people are falling out of bed but also that a correction of the attitude gives such a resistance. No research is done about these phenomena in sit or stand. Balance??
Robinovitch and his colleagues have found that most people in long care facilities fall because the weight shift isn’t correct. We need therefore assessed this perception (chapter 2).
Older people with increasing age loss also a great part of the input facilities and the interpretation of the brain must be alter. This differentiation is difficult to make but they are signs that the discrimination sense, the gnostic sense but also the vital sense are lesser or that the interpretation in the brain is lesser or both.
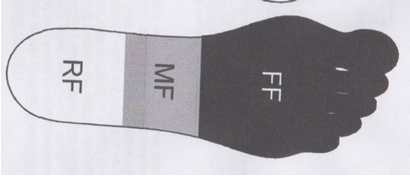
Prof. Duysens [61] from Leuven fond that the heel of the foot appear by elderly not the weight bearing point and an “feeling “point any longer. There is a shift to the mid foot and that means that walking with an heel strike isn’t used anymore and that will be give an change in the activation of the gluteal muscle and have consequences in the use of this muscle.
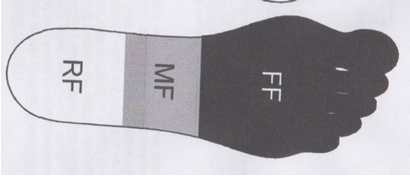
Figure 10.
The most weight was placed on the MF part and less on the RF part. That makes that the FF part must be part of the weight bearing task and has less room for feeling and fast corrections.
Clawing by elderly and especially by elderly with dementia is higher and especially that group of people with dementia that has an increase tone in the leg.
Clawing is an adaptation to create more stability under the feet and it is important that this clawing ability can be done. That must be a part of the treatment to hold this part in an optimal mobility.
This isn’t easy because tone increase and clawing goes often together. That high tone in the muscle can lead to a loss of sarcomeres and decrease of muscle length [62, 63].
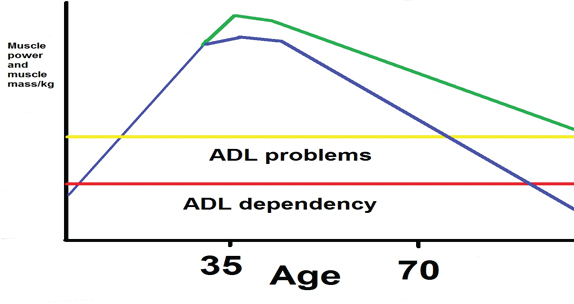
Loss of muscle power-Sarcopenia- has a direct effect on the possibilities to do the own ADL activities. People with dementia through the loss of cognitive functioning will have troubles to hold the control about the own ADL , but the loss of enough muscle power and coordination will contributed to faster loss of this part of their independency.
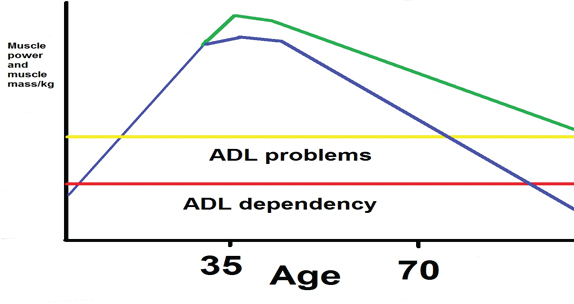
Figure 12.
Here we see what the decline in muscle power will do with the ADL independency. The turning point lies round the 35 years, then is the question how fast the decline is and also important what is there build up in the years before this turning point. Training has influence on the decline. The Yellow line is the line that gives an border for ADL problems, the red line gives the border for ADL dependency. The vertical axis gives the amount of muscle power and mass in kg. and the horizontal axis is the age line.
Sarcopenia is something, that can be present by everybody but:
- The amount of muscle mass previous is important.
- The way of live is important after the turning point, because a high mass before the turning point and after that a way of life without muscle training will not prevent that the line will go faster down.
- The clearness that enough muscle power is essential to hold your independency. Stair climbing is very important and this exercise every day will prevent that this decline goes faster.
Of course can a training program, this fast decrease slowing down and especially in long care facilities were often the amount of movement is very poor. The combination of Movement Guiding Care [66] and training program with task specific resistance treatment that fits the rules [67, 68] can slowing down this and prevent ADL dependency at a too early moment.
But there must also a good protein intake important and that is about 1.2-1.5 gram per kilo body weight a day. Still not all type of muscle will be survived, mostly the fast fibers will decline first and that will has and direct influence on the balance.
Creation of this scheme is [69, 70] done to protect this group of people because treatment asked always much from body and mind. Working in a Nursing Home, it was in the beginning a “culture shock”, that the physical therapist came on the ward to train this group of people. Many of our colleagues nurses had the feeling that we decrease the quality of life of this group, because they found that they had earned there rest and inactivity. They now care for them and they had the privilege to enjoy their stay on the ward. Starting with a treatment of the people in the foetal attitude, we convinced the nurses and other members of the team, that this way of inactivity isn’t the quality of life that elderly with dementia like.
The extreme tone that decreases has many “eyes open” and we all look to the other inactivity and the level of quality of life. The aspect pain was an great example, when we discover an man with often an behavior that was very unpleasant to everyone, that he suffer from an gout attack and when the medicament were given, this man change and was kindly and walk with you and help you with all kinds of things.
Therefore was the scheme important to see what someone can and enjoy doing with his remaining possibilities and how we can help him to stay as independent as possible.
But on the other hand this disease continue and when the possibilities are lesser, than it is very important to care for them with using the remaining possibilities but also with the view that what is very heavy is an training and that someone cannot do that whole day.
That means that the environment must give enough support to hold this dependency and when assistance was necessary than must that be done on such a way, that this people have the feeling that they can do it almost on their own.
This likes simple but that isn’t so, because now everyone must be have knowledge and skills about the motoric performance of elderly and elderly with an neurological disease as dementia and they must be trained in the techniques to approach this people from Realistic Orientation Training (R.O.T.) Validation, Dementia car mapping, Presentation, warm care, P.D.L. (Passive Daily Living), reminiscence, the approach of Anneke van der Plaats etc. [71, 72, 73, 74, 75, 76, 77, 39, 40], furthermore they must see what the border of their brain are, that we called Capacity.
Capacity means that people must act on an too high level and that can be both physical and mentally and when someone act on that level, the reaction will be always;
- Motoric signs as higher tone, walk away, fight, squeeze etc.
- Mentally signs as screaming, cry, don’t willing to listen, apathy.
Often this combination will give us and sign that something’s isn’t alright. Of course a lot of other reasons can be triggering this behaviour but as member of a team, it is our task to ensure that the physical condition isn’t the reason and that asked a good assessment and a connection with this individual.
We know that this is difficult but no connection with this people, will give a contribution to the quality of life of this group people, that minimal and often doing or suggesting things that will decrease the independency of this group of people.
The amount of active elevators and wheelchair that change the perceptual track and make movement almost impossible and/or wrong is so great. The reason to use them is to lower the burden of the care givers/nurses etc. and often is the patient the “forgotten” group. (More is chapter 4and 5)
Phase 4 (chapter 3)
The disease asked for an approach that we enter their world and often is that world of the past.
Reminiscence makes it possible to make contact and lay connection with movement out the past and create training. In this phase of the disease most people are living at home and must the therapist treat at home. That asked specially qualities because there is the person the “lord of the castle “and are you the invader. Special qualities are necessary and a good evident based approach. We use the EDOMAH –approach [78] that start with an inventory of the wishes of the person and his/her family. That is the starting point and makes it possible that the physical therapist as team member can stay and treat. Physic can start in this stadium, the focus lie on balance and walking capacity and that we will use to give an aerobic training with a good intensity to slowing down the disease. Balance training asked for more than only aerobic treatment because this is a coordination problem in which the correct amount of strength and speed are necessary to control the balance.
Here the assessment is essential, because in this phase can it be that the problem is the changing tone. Still by many elderly it are muscular failures that are present for years and now is the system at the end of his adaptation and fail this system. An assessment (Chapter 2) can give clearness of both. The loss on cognitive function makes not that people fall more, but make that people were afraid to move and therefore loose more muscle than necessary and that is reversible.
This isn’t by everyone because you have people that likes to move and sport but there are also people that hate it. And by then this will be difficult and asked a special approach.

Photo 1
He has suffer from an hernia that has decrease his power in his left calf muscles and makes an push-off, that is not enough. Through the push with the stick in his right arm/shoulder, he stimulated his back diagonal [80-84] to equalize that. That makes that this is an action on the border of his function and we see that he has bend his head to see the world direct in front of him.

Photo 2
Man with dementia, living in a Nursing home, because his behavior was so difficult that he couldn’t stay at home. He walks the “whole Day”. He wasn’t very friendly to the other people. He fall frequently and everyone try to get him walk with a rollator frame. But that aid was often “forgotten”. Nobody had tested him on his balance performance and there are on this picture signs that balance can be a problem. The bended elbows must give us and sign that he has too much power in his upper trunk to control his attitude and balance. Assessment is than necessary and not only a BBS [46].That was 38, too low, but why?
Photo 2 is good example what we can expect in this moment of the disease. Often there are other problems that have the greatest impact, why people move to an long car facility and the most common reason is that troubles at night and that is for the care-givers isn’t to endure any longer.
When such a person is transfer to a long stay facility, than is it important to assess. A BBS–test isn’t enough because we know that he can fall easy but not why.
On the photo we see two elements:
- The bending elbow as an sign that he has more tension in his shoulders, to have more control over his back diagonals.
- He looks in front of him instead of looking far forward, to see what for obstacles there are.
Investigation of the multidisciplinary team gave the next results:
- His eyes were poor and the amount of light was bad in the corridor and in the room he visited and lived
- His power in his buttock muscle was decreased and he wasn’t capable to react on balance disturbances on the right manner and with the right speed.
An training program give an fast result, because he enjoy exercising as he was an great sportsman in the past and the tension in the elbow was less and also the amount of falling decreased.
His BBS alter a little bit from 38 to 41.
The other members of the multidisciplinary team came with their results:
- Blood assessment because the relation to light inflammation and lesser balance is known. And out this assessment was clear that here was an infection of the bladder that was there for a long time without temperature changes.
- There was also an investigation of his eyes and was not so good [86, 87]. The examination was done by an eyes specialist and through the CORVIST test (Cortical Vision Screening Test). He gets glasses but he need time to get use on this. In the main while the light possibilities were increased on the corridor and in the rooms he visited and the railing were painted in black. [88]
All this intervention had an amazing effect, what nobody had expected.
He sleep better and was changing in a unfriendly man in an friendly man, that search for others for contact and has helpful with all kinds of work.
He walks better but mostly closer to the railing and often with a hand light on it.
His amount of falls reduce to zero
His BBS was improve with great exercise effort to 44, but with the others inventions he goes to 46 and this is the improvement from 38-46= 8 point and that is a significant positive effect.
This is too important because we think that a loss of coordination is the reason but all elements have influence on each other and to work with each other we can make the quality of life much better. The personal complaint that when he goes to the toilet, he often urinated not in the toilet but closed to it on the ground. We now give the toilet-lid a dark colour and we allow him to go to a toilet with on one side and wall and now go “all in the toilet.
People with dementia are often forgotten through the other medical specialist, because the diagnosis dementia seems to be a “curse” and all other things are not necessary.
But people with dementia will not fake that there is something wrong, but the will not reported it.
Not be well isn’t something that and person with dementia will say but he show it to you.
The problem is that this showing must be understood otherwise we miss the signal.
Now independent moving is be growing difficult. That can be through the age and the disease but this can also be suddenly often through a fall with a hip fracture. Fall prevention will be an item that is introduced at the beginning with balance training but this is an degenerative disease by people with an age from which we can expected that moving is difficult and that will give almost certainly an fall. A fall and especially a fracture give every time a moment that everyone taught: “This wasn’t so bad, she/he is walking again “.
This is always a rare moment. People with dementia walk often faster after a surgery by a hip-fracture as people of the same age without dementia. This has something to do with their reaction on pain of better the lack of the expression on our way. The lack of pain expression and the desire to move are often elements that both therapist and caregivers give the impression that this going fast in the good way but watches what you are seeing and hears:
Look to their. Face the tension on it and listen to the breathing. Sign that this is very difficult and heavy, that is their expression of pain and great effort. [54, 55, 89]
The behavior is often different. We know why because it is obvious after so event. But this give also a sign that this people are working above their mental and physic capacity and that will have consequences. The reaction will follow therefore, try everything to brace the extreme movement wishes or make all easier.

Photo 3
When this lady takes weight on her left leg and swing their right leg to the front, both front wheels turn to the left and that is a sign that standing on the left leg askes for more support. That support is increase by an upper trunk lateral and pushes the rollator frame more to the left. This movement must she brake at the moment the shift is complete and the right leg goes in the standing phase and then the wheels turn back to an straight line. This movement must be controlled in their shoulders and especially the left shoulder will have a hell of a job. This makes walking very intensive and there be must be sure that this intensity isn’t too high.
This we can measure by walking with them and observe and talk because often the stand still because two tasks is too difficult but this say something about the mental capacity and not directly about the physical capacity[92] .We can also measure the saturation and especially the heart rate frequency. Intensity scale [94].
All people after this use aids and rollator frames. Again obvious but this gives us and sign that weight bearing without support isn’t possible anymore. What we not known how much support she takes. We see abnormal movements, signs of Trendelenburg [90] and Duchenne [91] but we get no information directly how heavy walking, standing and standing up is, therefore watch the face and listen to the breathing. And do a regular inspection of the palm of the hand and the mobility of the shoulder joint. Watch when the walk what the rollator frame do, often the straight forward movement isn’t there and make the front wheels all kinds of movement lateral and that asked much from the shoulder muscles to control that. Decrease the amount of walking and look to their face and listen.
Last point that often underestimated and that is the reaction on the narcosis [94]. This had an effect on all cognition of older people but people with dementia have lesser capacity and this will have a greater impact on their mental/physical capacity. And this capacity is all under pressure through all the changes and burden there are having. We see that after an month their mental capacity is decrease and sometimes heavy with all kind of signs mentally but also physic and one of the most signs is the increase of pathological tone and the occurring of pathological synergy that makes walking, standing and standing up far more difficult.

Photo 4
Walking independently in the corridor. All attempts to get her on a rollator frame fail. She walks in the corridor and always with the support on the right hand/arm. Therefore was necessary that she crossover to the other side but she find a way that this was done easy. Walking under supervision gave a much higher heart-rate and we must see this as therapy and not what we want the whole day. Here she had the possibilities under control and enjoys the walking but by the rollator frame was the intensity to high that it was an aerobe exercise. With the railing she was in control, with the rollator frame laid the control elsewhere and was it every time an exercise.
Please, give all corridors and give a good railing system, it is in many ways the best option for elderly and certainly elderly with dementia in this phase. She can than more in control and independent, often with the rollator frame are we the people that decided the speed.
People with dementia that functioning at the border of their capacity will less cooperated and will often refuse to exercise. This always must walk to the end of the corridor; every day will change their behavior because they feel that they are failing. Failing [39, 40, 41, 42] has an negative effect on people with dementia and will decrease their quality of life. Laughing and other pleasant activity has the opposite effect [95]. This always functioning on that high level is something what must be lowered and then exercise to improve some element is possible.
To achieve this, many use a form of motoric learning. Motoric learning is a strategy that is used in this phase to “learn” this people another an “better” way of moving, as par example error-free learning [96]. In the phase 4 certainly progress can be expected with this and other approaches but in this and the latter phases is this almost not possible because the loss of mobility and power is to great and that is the problem. Their procedural memory is often intact and the brain helps the body to move with the possibilities it have and our job is to find an way to help this system to move within the borders and create an new equilibrium in which the people can move within their mentally and physic capacity. This asked for knowledge and skills to observe how elderly with dementia move, what their reserves are, they have and how we can use that to create movements with the greatest possibility to do it on her own.
But the reality is different, regrettable we often help so fast that this possibilities are minimized and the environment is often more difficult for this group to hold their own possibilities. There are sign that the brain also “learn” wrong of this approach and that this one of the reasons that walking and falling will occur more. One of the most common reason that elderly in long care facility fall is an wrong weight shifting [97, 98]and there are sign that this not only count for walking but also for standing, standing up and sitting. We have mention the lying attitude that is oblique and that perceptual change can also be present in standing and sitting position and they are maybe make by the way we “help” them or create situation in which we use elevators to get them in an standing position.
We know that though the damage in the brain their body perception changes but there are little investigation what will happen when this people are brought in an attitude that is in wrong equilibrium. A wrong way of standing up will create in the brain a new perceptual track.

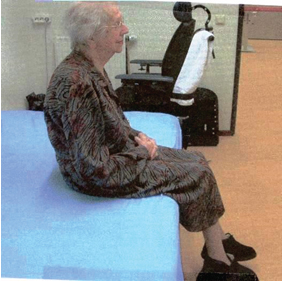
Photo 5
This gentlemen show something that is typical for phase 3. Standing up with arms pushing on the side support of a chair. This chair is higher than normal still this strategy is use by elderly when the power in the legs is too little. But this ended always with a border! He stands out of balance because his feet stand to far in the front and the support stay on the arms. He must now take a risk to try to get a support on the bench. And then can glide the chair away and when this attempt is fail he fall on the floor. This strategy we teach elderly as a safe standing-up strategy but all “normal” rules are neglected. The procedural memory knows how he must perform but the power in his legs is too little. Still make the environment correct and the system have immediately the solution.
Here lies am problem that it isn’t an problem of “not-learning”- capacity but the problem is that this strategy isn’t usable when the power in the legs are too little.
Often this strategy fails and then we use a support (Photo 6)
We assume that their procedural memory is not intact and we try to teach a better way to stand up but we are wrong. This way of standing up is a sign that the power of the leg isn’t enough to stand up without the influence and power of the arms. But we make the situation so bad that this the only way they can stand up and forget that when the body isn’t moving to the front far enough the procedural memory cannot act as it should be.
Elderly must go further to the front to get the system working and that asked something in front of them to support. To go so far to the front with nothing in front will no elderly do and learn that is nonsense. But help (photo 6) or sustain that strategy (photo 5), is creating a wrong perceptual track that will place the equilibrium “behind the feet”.
The sign of falling back-dorsal flexion of the feet- is still there on photo 6, but latter on we see that this reaction is lesser and sometimes not visible anymore. Stimuli that enter the brain, even an damage brain, make an projection not only on cortical level but also on lower level [99, 100, 101] This projections must be feed with much stimuli and that is the greatest problem because this stimuli that now be given are continues the same and wrong and with change the body perception and also the balance perception and we see often after an few months that the muscular reaction that must be there by an balance problem isn’t active on the right moment. The conclusion of Robinovitch and co [97, 98] that the weight shifting is not right and thus also the reaction, will be make movement and certainly independent movement much more difficult and will decrease the quality of life further.

Photo 6
Analyze this photo: What must this lady do to get her body in upright position. She starts with pushing up with the arms and that can only at this moment. Moving further to the front makes this pushing up more difficult. The nurse pushes their shoulder against the person to the front and that give as reaction from the lady a movement with her shoulder to the back. This gives an upper trunk –left –to the back and in the diagonal [80, 81] her right foot will be place further to the front to help the movement to the back. What we further see, is that her brain feels that the equilibrium isn’t good, because the balance reaction in the forefoot is present. But when everyone on this way gives assistance. Than is the expectation that this foot-reaction isn’t present anymore.
The brain has learnt that the “balance support” is large as the foot and goes further behind the heel.
The brain has created a new perceptual track that isn’t equal with the reality!!

Photo 7
Photo 5 and 7 are the same person on the same place at the same time. The red chair is 10 cm higher than the blue chair. Photo 5, he stand up as must do on the ward and came not further as that. He needed assistance to get up and take his rollator frame. Photo 8, he may use the bench in front of him and we teach him to place the whole underarm on it with a bended elbow. That is far to the front but because of the bench, he dares to make this moment. This is an important fact!!
By photo 5 and 6 there is no support in front of them and that can be the reason that elderly this strategy must use (photo 5), because there are no other options. The environment isn’t optimal for elderly, look around!!
But compared photo 7 with photo 9 and what is the greatest difference!!
What often is taught that elderly lost their ability to standing up because the know not how, ii is done. Normally will a good movement of the trunk to the front by everyone, who want to go stand, give in the knee bending and the feet are placed behind the knee, still in sitting position. Nobody think about this but this occurs because the trunk goes far enough to the front and this occurs when the feet are not weight bearing. He (photo 7) does the same, goes far enough to the front and the reaction occur automatically, the feet goes to the back and stand perfect!
Thus this problem of standing up isn’t an problem that the brain don’t know how but the power in the leg is to little that the arms must help and now can the trunk not further to the front and will the placing of the feet not be complete.
This is the main problem in this phase, there is no possibility to use an strategy to create this way of standing up because the leg power is too little and an good fixed support can change that and now has training of the leg muscle an extra good effect because this way will be easier.
Chapter 2 will show how to asses and the gentlemen will serve as an example in the explanation of the assessment.
Photo 8 presents the geriatric chair!!

Photo 8
Photo 8 show what many elderly have, a trunk that has lost his length and that can be huge. The legs of both ladies are equal of length, not of form and muscle power and tension.
But this geriatric chair has a support for the neck on a height of someone without loss of length of the spine. The armrest sits to height for the older lady. The sit angle is on the back-end lower and that makes standing up and moving in the chair difficult and together with the height of the chair (to low) makes it standing up more difficult as has to be. When this lady sits on normal chair on normal table, she will have great troubles to eat on that table. Still never say we chairs and table that are made with the adjustment to copy with the loss of length in the trunk.
In this phase of the disease be alert that the environment is fitting and that this environment helps to hold the independency. This important because the disease goes on and the problems to move on their own are getting bigger and asked for solutions that serve their mobility first. Still one of the elements that we see change is that the walking ability isn’t good enough to come from the room to the dinner table etc. and we see the wheelchair.
Observe when someone can sit in a normal chair but is transported with an wheelchair, how fast he sit the whole day in the wheelchair also on table. The number of transfers and movements are than only 20% of the transfers and movements that this person was making when he was transferred each time out the wheelchair in a normal chair. This will have an influence on the person, his mind and his body power.
Of course will the mental- and body capacity decrease to a level that walking is so heavy that it is the heaviest exercise there is and that must be avoid. That is for the physical therapist to exercise and his accent must lay on the possibilities that are asked for the ADL and care. Therefore less walking with a rollator frame, but much more accent on standing up, standing and task specific resistance therapy to support this. Walking with a rollator frame will now have little interest because it isn’t use anymore. Walking a little distance behind a chair or walking side way along a table is much more functional. Often this great amount of variation [102, 103] is the best way to stimulate the damaged brain to search in their possibilities of the procedural memory, and when we want to exercise on a higher and more variated level than we must change the environment and especially the influence of the gravity. [104, 105]. Go into a swimming pool and be surprised what all will happen. Because that gives much more information / perception [106, 107, 108] to brain and makes the burden of the body less heavy [109]. And this will have influence on their cognition [104, 110] but also on their behavior and sleep rhythmic.
This can be done in all phase, of course. And give people an pleasant day and is full of ADL etc. and has an great aerobe an anaerobe component, there cases that people even in phase 1 let surprising things seen.[111] Still the most day this people are on the ward and regrettable often the whole day in the wheelchair. When there is a transfer possible and sitting in normal chair is good possible, make the transfer on a good way according the normal movement that elderly make and always in the right balance situation. Prevent that this people learn an wrong perceptual track that often now occur by using all kinds of active elevator that pull this people on the upper trunk up with the feet never in the good position. This will lead to people that not dare to move to the front and in sit, they will move to the back and that can even have an influence on the swallowing capacity [112].
The investigation that has recorded the action (coordination) and the muscle power height [113] gives there a clear example. But the greatest lost is the perceptual track change that “push” this people to the back and make movement and lot more difficult but also very anxious.
They are afraid to move to the front an often the sit on the edge of the bed out balance.
Photo 9

Photo 10
Photo 9 and 10: We know that the body perception is changes in a lying position often around the 7-15°. Often in Phase 3 but certainly in Phase 2 when sitting is the major activities that people do through the day, we see this picture. People that sit too far to the back and often search for security. Photo 10 here is an battle with the reality and that hands are used to secure the situation.
And by this position we will see always an extension of the leg. Movements to the front are stopped immediately and with great fair of falling to the front.
That position in the wheelchair, the whole day , because often is resting on bed replaced in an sleep moment in the wheelchair that is placed in an back stand, give us the feeling that movement isn’t important anymore. Still -movement- it is the only possibility to stimulated the brain and the body and when the brain isn’t stimulated, will the behavior change but also the body. Muscle will decrease in strength and coordination, tone will increase, pathological synergy will occur and that lead to a greater danger for contractures [114, 115] and that can lead to pressure scores.
A great game on a table [116] to get more attention, quality of life and movement on the table by people with dementia. But on this table there is only one person that can play the game with great “reach”, the others have restriction because the chair is stand in an “Nursing Home stand” to close ‘under” and very close to the table and the woman in the wheelchair cannot reach because the leg rest stand up and that gives an stretch on the backside of the leg and nerve tissue [117, 118, 119] and for three person the table is too high!! There is no possibility to support on the elbow!
At the stage the danger of pressure scores is present and scientists are looking how to decrease this risk. Regrettable not a search how can the person move better en create on his own a lower pressure. But how to create a sit position with an equal pressure that is low and the person can sit almost the whole time with a minimum on pressure score. Is this quality of life or create a situation that this group of people has less support of professional needed!!
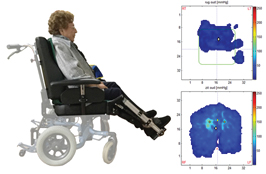
Photo 11
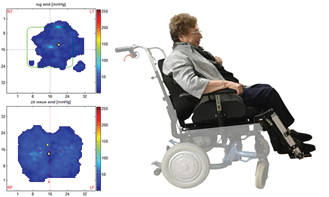
Photo 12
Photo 11 and 12: A change of sit attitude and in this called: “active Sitting “. The important issue is to decrease the pressure around the tuber ischia. Photo 11 rights under is this visible in the light blue part where the pressure is high and dangerous. Therefore this person will suffer and that is the reason to make another construction. It curious that still so little people search for an attitude that makes movement possible and create much more movement [121, 122, 123]. Photo 12 gives the result another sitting posture with not the light blue pressure marcs around the tuber ischia. The danger is gone, case closed! But is their moving capacity increase? Photo 11without the leg rest so high and with a sitting horizontal, we need than a table in front of their and she can move to the front and decrease the pressure around the tuber.
And there is another problem that will have a huge influence on the quality of life. This sitting posture together with the sitting back creates an antero position of the head [64, 124].
Movement is essential for the quality of life, mentally and physical and long sitting isn’t one of them. That older people sit more is obvious but let’s be honest, in most long care facilities it is usual that people sit for more than 4 hours without standing up. That is much too long, to prevent pressure score is movement each 2 hours necessary.
Photo 13 show a picture in which this “quality of life” gives a face. This lady had great difficulties with eating at their own, because she wasn’t able to use a spoon through the decrease power in the arm and the pain. The solution is than obvious we help her.
But was it necessary, have we create a wheelchair that this has influence on the movement possibilities and even can hurt. Her amount of independent movements are zero, all movements/transfers are done with a passive elevator. Even the elevator sling is still present and we know that this done everywhere, still will this have a negative effect on the sitting but also of our idea about fatigue of the person. (Chapter 5)
But after an assessment we discover that here mobility, power loss has a clear reason. She had an cervical- and lumbar stenosis [125], that means that when she sit with leg rest up the whole nerve system stand on tension and that hurts and restrict movement of arms , head etc.

Photo 13
Some people had commentary on the way the nurse gives the lady food, too high! She must lower their hand and stimulated so that the patient makes the neck long on the back side but this chair with the extreme leg rest makes this for this lady impossible without pain through the whole body. Cyriax [126, 127] has this called spinal cord signs and pain that can come everywhere, but in this case was also the cervical spine restricted and give this chair an partial paretic m. deltoideus through an “restriction” of the n. axillaries and that was the reason that the arms don’t were able to hold an manipulated an spoon.
Phase 2 asked from us that we search for all possibilities that people can move and the best movement are the movements in direct connection with the A.D.L. All transfers in an out the wheelchair are so important and give a person a higher quality of live. This askes from all professionals knowledge and skill about transfers and makes the physical therapist and trainer and a teacher. When the tone is pathological as by all severe neurological diseases and the signs that the body must function at the border of his brain and body capacity, must this be recognized. The static reaction [128, 129] that often occur when this people must work on the border of the capacity are often not recognized and then is often the disturbance of their behavior not understandable.
Special the Foetal attitude with a high tone is the most bizarre attitude. This is an attitude that we only see by patients with and sever neurological disease, gives us a clear answer where we Dementia as illness, must place. It is a severe neurological disease that damage in the brain is gigantic and that not only on speech and memory but all brain function will be damaged.
We have in the phases for this last stage see that movement plays an important part in the slowing down of this disease and that is through the amount of stimuli that forces the brain to search for solution but this damaged brain has need for stimuli that helps it to create this optimal climate.
These stimuli must have a dynamic character [39, 40, 130] to enter the brain, but also to achieve more than only a moment of change. Dynamic exteroceptive/proprioceptive stimuli will enter the brain and will give not an immediately extinction phenomena.
That count for all phases but in this last stage, is this more difficult because movement will lead to a kind of disturbance that many people find “unhuman”.
This means that we must search for equilibrium between that. Because dynamic stimuli can give a behavior that is restless but the same stimuli give also a normalization of that unpleasant behavior and tone. This is also the case by people in the foetal attitude, dynamic stimuli can decrease the tone and increase the few cognitive possibilities but nobody can tolerate the whole day dynamic stimuli and that asked for a scheme and a good multidisciplinary team.
Hypothesis [131]: Why goes someone in a foetal attitude with a high tone??
Stability is the key element that has so much influence on the body and the brain. The “unsafe” information that this damage brain receive, set this brain on work with all it has. He makes the tone as high as possible and search for a central fixed point and use the strongest muscle pattern that there are, that we see by all severe neurological diseases. The static reaction [14, 15, 128] are used to get the best stabilization and we see often in this phase, the general static reactions. They originated from the head or through sense- (par example vestibular) system in the head. Therefore be aware when the tone is high in the head and that can MAS-P 4. That is the highest score that can reach and then is almost no movement passive possible [132, 134].
This has consequences, this high tone will consume all brain activity of this person, often there is no contact possible and their eyes are don’t “looking”, this person is in total other world.
But when we try to give the brain information that there is enough stabilization and the damaged brain recognized this information than will this brain lower the tone and often we see than what cognitive reactions.
Crucial is the tension in the head!!!!
Often are the interventions nice and give Nan symmetrical bed-attitude but the relaxation of the head isn’t there and then is an intervention that is not reaching the brain. Tension in the head in extreme extension is so pathological that this must be the leading item where our intervention is based on! And we observed when this extension is increasing and that can also in previous phases, than is that and sign that there is no enough stability. Start with an assessment and measure the tone of the whole body but especially the tone of the head. There will extension create a tension through the back diagonals and create a flexion synergy in the shoulder (retraction scapula) and an extension synergy in the legs (high tone especially in the adductor muscle).
Look where he is place on:
Lie he/she on an soft bed, than will this bed give no stable information. Often lie this people on an bed that has an anti-pressure score system with air-pressure system and it is interesting to see what’s happen when this bed is complete filled with air and is hard. When the tone lower within one hour than this is an indication that the supporting area was to soft.
Of course is the risk of a pressure score present but a soft bed and long-time has also a great risk and maybe higher than a hard supporting area and a short time [135].

Photo 14
A great game on an table [116] to get more attention, quality of life and movement on the table by people with dementia. But on this table there is only one person that can play the game with great “reach”, the others have restriction because the chair is stand in an “Nursing Home stand” to close ‘under” and very close to the table and the woman in the wheelchair cannot reach because the leg rest stand up and that gives an stretch on the backside of the leg and nerve tissue [117, 118, 119].and for three person the table is too high!! There is no possibility to support on the elbow!
But important is that there is a decrease of tone and that means that the brain is working so hard to get an optimal stabilization. This and the position of the head, place the head-rest never flat are basic elements to create a stable situation. Still the danger of pressure score is still present and we must see of this lead to movements that prevent this or that we must change the attitude with a frequency to hold the good support with the decrease tone.
Often stand the bed in the mid of the room, strange because that give the person when he has possibilities with his eyes or even arm no opportunity to see or feel where the borders are of his environment. Be aware that the eyes are often not so good anymore, and a ceiling with has clear marks and when it is possible let this move because that is a dynamic exteroceptive stimuli. Often we see this people lying in bed with on the wall behind them the photos of their love ones and the only person that cannot look at then is the patient lying in bed. Place the bed always with one side against the wall. Not only in the phase but in all phases. The placement of the bed in long care facilities is again a sign, that it must be easy for the nurses but in this case it is very difficult for the person lying in bed to orientate himself.
These two elements are the base of a good intervention and are very important. Often is there a lot of interventions done but the base isn’t there, than will the tone in the neck not going down.

Photo 15
The foetal attitude with the typical posture of the legs. But look to the head and see the extreme extension of the head and the tension on their face. Here is someone working to create the best stability. That extreme tone in the neck and that face expression must be change when we want an intervention call successful.
Neck extension is therefore very important and will create a high amount of tone in the back diagonals and therefore a retraction in the scapula and that is the beginning of a flexion synergy that makes washing and dressing so difficult. ( An flexion synergy is the poorest attitude synergy that there is, because the neck extension in combination with the back diagonal create an extension in the spine muscles also is there an base for only an flexion attitude synergy)
But these back diagonals create also an extension synergy in the legs. There is a lot of flexion in hip and knee and there is a great resistance in this two joint to extension but still it is an extension synergy and the amount of tone in adductor muscle and the joint position especially in the hip decided what amount of flexion we have.
But important is that the legs were stabilized because now the rotated to one side and that will create more instability and there more tone [137, 138].
Sometimes is a good support, the head-rest a little bit up and a support under the legs enough to lower the tone, but then we must have a tone of Mas-P 3.
There are also patient that has an high tone when the sleep but when the awake than the start to move and decrease the tone but when the stop with this movements than often the tone increase and this group moves the “whole “day to hold control over this tone.
Here is not the stability the problem but the extinction. When the brain get not enough information goes the tone up.
This problem will we have with all our patients because when they are not capable to move on itself than will the amount of input decrease and will the damaged brain the tone increase.
All intervention will have that problem and that asked for an individual approach and schema in which also the pressure score prevention is a part of this.
When the assessment of the tone is the measurement on which the intervention are connect that we can give intervention that are enough to get an positive effect and know we what we have done and when this intervention has loosed there purpose.
Too frequently is our experience that an base intervention is done and that everyone see that this “looks good” but there is no good recording when the tone is increasing. That this occur is normal through the extinction but what is than to be done. Mostly will the tone be extreme in the morning because the last part of the night are the less attitude changes done but makes the morning care extreme heavy.
A good schedule with every time a good tone assessment is essential to get the best result and not only on tone level but also on cognitive level. That can give us the opportunity to get the morning care on much better level, but also the moment of eating and visit moments from the family etc.
Feet and hand have need of input that is firm and that is dynamic but the whole day dynamic is exhausted, therefore make an schedule as dynamic stimuli are necessary to lower the tone at his most and know that after that the tone will increase because the dynamic isn’t dare anymore [140, 141].
There are some patient that search for that dynamic, but by most there must be a stimulus that provoke that and create dynamic stimuli through movements. Par example the pushing away orthosis because this gives a feeling of discomfort a pushing away is than the answer and that lead to a tone decrease especially of the neck upper trunk and from the legs (Chapter 6)

Photo 16
Here we have done everything to create the optimal stabilization “feeling “for the brain and create a lower tone that was Mas-P of 4 to a Mas-P=2.
The hand had firm roller and they felt out her hand because she open the hand spontaneously and that occur when the tone in the head was low (Mas-P= 2) and that occur when she push away the orthosis with their feet and upper legs. But that where moment of 10 minutes that she generate that self, when we want to lower the tone we place an pillow under the orthosis and create more pressure on the legs.
Be aware that every treatment must have an individual component and then is a good assessment necessary. We realize that this is difficult, certainly in the phase 2 and 1, but better in phase 4 and 3 and tone measurements are always possible.
That this tone change can occur in the beginning of the disease is well- know, but then is measurement essential.
When the tone is increase, pathological synergy will occur and the selectivity, perception will change and decrease and then is an important because the exercise must count with that.
With an increase tone is task specific resistance therapy still possible as anaerobe training but the reaction will be lesser. This cannot change because the speed will never get on the proper level an essential part in the balance training. In chapter 3 will this discuss and one solution is working in the water, because water inhibits the gravity and thus the tonus. And it gives aerobe stimuli and that are still today the best possibilities to slow down this neurological disease [142].
The Chapters 4, 5 and 6 will focus on the decreasing of functioning and the possibilities that are present through task training and environment with an multidisciplinary team to hold the self- independency so long as possible at an high level and will also focus on the quality of assistance to give the person the optimal possibility to use his own possibilities!!
This with the purpose to hold the quality of life at its high possible level.
Authorship credit: “Criteria authorship scientific article” has been used “Equal Contribution” (EC)
- Matthew W McDonald, K Rosbergen, Jeffers M, et al. (2018) Is Environmental Enrichment Ready for Clinical Application in Human Post-stroke Rehabilitation? Front Behav Neurosci 12:135. [Crossref]
- Neuvel K Petit, Kooistra M, Steinbusch H (2015) Alzheimer onderzocht. Lannoo Campus.
- Scherder E (2017) Singing in the brain. Athenaeum –Polak$ Van Gennep.
- Aleman A (2017) Je brein de baas. Atlas contact.
- Aleman A (2013) Het senioren brein. Atlas contact. ISBN 9789045019826.
- Ramakers I, Boesten J, Visser P, et al. (2007) Symptoms of Preclinical Dementia in General Practice up to Five Years before Dementia Diagnosis. Dement Geriatr Cogn Disord. [Crossref]
- Hausdorff J, Hillel I Shustak, Del Din S Bekkers, et al. (2017) Everyday stepping quantity and quality among older adult fallers with and without mild cognitive impairment: Initial evidence for nem motor markers of cognitive deficits? The journal of Gerontology.
- Michikawa T, Nishiwaki Y, Takebayashi T, et al. (2009) One-leg standing test for elderly populations. J Orthop Sci 14: 675-685. [Crossref]
- S Ryerson, K Levit (1997) Functional Movement Reeducation. Churchill Livingstone.
- van de Rakt J, Mc Carthy Grunwald S (2016) Diagonals Part four–Stroke 2 Transfers in bed and the chain rules. Ita J Sports Reh Po 3: 616–669.
- Kraft P, Gadeholt O, Wieser M (2009) Lying obliquely-a clinical sign of cognitive impairment: cross sectional observational study BMJ. 16: 339-b5273. [Crossref]
- Hobbelen JS (2010) Paratonia enlightened. Definition, diagnosis, course, risk factors, and treatment. Proefschrift. Enschede, Gildeprintdrukkerijen.
- Van Deun B (2018) The impact of paratonia on fine and gross motor function in older adults with mild and moderate dementia. Alzheimer Dis Assoc Disord 33: 54-61. [Crossref]
- Davies P (1999) The comprehensive treatment of patients with hemiplegie. Second edition. Completely revised and updated. Springer-Verlag 3: 540-60720.
- Bobath B (1079) Hemiplegie bij de volwassene: evaluatie en behandeling. Bohn, Scheltema& Holkema.
- Barnes M.P & Johnson G.R.(2001) Upper Motor Neurone syndrome ans spasticity.Pag. 12-71. Cambrigde .
- Howle J (2003) Neuro-Developmental Treatment approaches. NDTA.
- Bassøe GjelsvikB (2002) Form und Function. Thieme.
- Van Cranenburgh B (1998) Neuropsycholgie. Elsevier gezondheidszorg.
- Kaas J (1999) The reorganisation of sensory and motor maps after injury in adult mammals. J Cogn Neurosci.
- Recanzone GH (1999) Cerebral cortical plasticity: perception and skill acquisition. Cogn. Neurosci. 24. 237-251.
- Bauman, Gillis K (2017) Brein Zorg. Acco.
- Van Cranenburgh (2004) Neurorevalidatie. Elsevier Gezondheidszorg.
- Stockmeyer S (1967) An interpretation of the approach of Rood to the treatment of neuromuscular dysfunction. Am J Phys Med 46: 900-961. [Crossref]
- Yekutiel M (2005) Sensory re-education of the hand after stroke. Whurr Publichers London and Philadelphia.
- Rueda Delgado, LM Heise, KF Daffertshofer, et al. (2019) Age-related differences in neural spectral power during motor learning. Neurobiol Aging 77: 44-57. [Crossref]
- Fallah Tafti F, Watson F, Blaskewicz Boron J, et al. (2019) Strength of plantar- dorsiflexors mediates step regularity during a high cognitive load situation in a cross- sectional cohort of older and younger adults. J Geriatr Phys Ther 16: 10.
- Gennaro F, De Bruin A (2020) A pilot study assessing reliability and age-related differences in corticomuscular and intramuscular coherence in ankle dorsiflexors during walking. Physiol Rep 8: e14378. [Crossref]
- Le GoicM, Wang D, ChiarovanoE, et al. (2018) An Initial Passive Phase That Limits the Time to Recover and Emphasizes the Role of Proprioceptive Information. Front Neurol 9: 986. [Crossref]
- Ellmers T Cocks A, Young W (2019) Evidence of a Link Between Fall-Related Anxiety and High-Risk Patterns of Visual Search in Older Adults During Adaptive Locomotion. J Gerontol A Biol Sci Med Sci. [Crossref]
- Erickson K (2012) Physical therapy, Brain plasticity and Alzheimer disease. Arch Med Res 43: 615-621. [Crossref]
- Netz Y (2019) Is There a Preferred Mode of Exercise for Cognition Enhancement in Older Age?-A Narrative Review. Front Med (Lausanne) 6: 57. [Crossref]
- GheysenF, Poppe L, De Smet A, et al. (2018) Physical activity to improve cognition in older adults: can physical activity programs enriched with cognitive challenges enhance the effects? A systematic review and meta-analysis. Int J Behav Nutr Phys Act. [Crossref]
- Hossien Batouli S, Saba V (2017) At least eighty percent of brain grey matter is modifiable by physical activity: A review study. Behav Brain Res 332: 204-217. [Crossref]
- Angelica Miki Stein, Thays Martins Vital Silva, Flávia Gomes de Melo Coelho, et al. (2018) Physical exercise, IGF-1 and cognition. A systematic review of experimental studies in the elderly. Dement Neuropsychol 12: 114-122. [Crossref]
- Marie Pier McSween, Jeff S Coombes, Christopher P, et al. (2019) The Immediate Effects of Acute Aerobic Exercise on Cognition in Healthy Older Adults: A Systematic Review. Sport Med 49: 67-82. [Crossref]
- Bossers W, Van der Woude L, Boersma F, et al. (2015) A 9-Week Aerobic and Strength Training Program Improves Cognitive and Motor Function in Patients with Dementia: A Randomized, Controlled Trial. Am J Geriatr Psychiatry 23: 1106-1116. [Crossref]
- Bossers W, Van der Woude L, Boersma F, et al. (2016) Comparison of Effect of Two Exercise Programs on Activities of Daily Living in Individuals with Dementia: A 9-Week Randomized, Controlled Trial. J Am Geriatr Soc 64: 1258-1266. [Crossref]
- Van der Plaats A (2008) De wondere wereld van dementie. Elsevier.
- Van der Plaats A, Kist D (2016) De dag door met dementie. Kroese kits uitgeverij.
- De Boer G (2016) Die past hier niet. Breincollectief 32-67.
- Geelen, van Dam H (2016) Dementie; Van hersenlagen tot omgangsvragen. Bohn, Stafleu, Van loghum.
- Groot C, Schwerder E, (2016) The effect of physical activity on cognitive function in patients with dementia. Meta-analusis of randomized control trials. Ageing Res Rev 25: 13-23. [Crossref]
- Hoffmann TC, Perera R, Altman DG, et al. (2016) Better Reporting of Interventions: Template for Intervention Description and Replication (TIDieR) Checklist and Guide. BMJ 78: 175-188. [Crossref]
- Pogrebnoy D, Dennett A (2020) Exercise Programs Delivered According to Guidelines
- Improve Mobility in People with Stroke: A Systematic Review and Meta-analysis. Arch Phys Med Rehabil 101: 154-165. [Crossref]
- Berg WP, Alessio HM, Mills EM, et al. (1997) Circumstances and consequences of falls in independent community-dwelling older adults. Age Ageing 26: 261-268. [Crossref]
- Franchignoni D (1997) Trunk Control Test as an early predictor of stroke rehabilitation outcome. Stroke 28:1382-1385. [Crossref]
- Mirelman A (2020) Tossing and turning in bed. Movement disorders.
- Zhao Y (2010) Progression of Parkinson disease as evaluated by Hoehn and Yahr stage transition times. Movement Disorders 25: 710-716. [Crossref]
- Rikli R, Jones C (2002) Senior Fitness Test. Active aging 1-30.
- Kang L (2017) Timed up and Go test can predict recurrent falls; a longitudinal study of the community-dwelling elderly in China. Clin Interv Aging. 12: 2009-2016. [Crossref]
- M Koolstra, I Burgers, J Lemmens, et al. (2001) Klinimetrie na een beroerte. NPI/VU Medisch centrum.
- SchädlerS, Kool J, Lüthi H, et al. (2006) Assessments in der Neurorehabilitation UItg.Huber.
- Sgro G (2016) Pain assessment in elderly with behavioural and psychological symptoms of dementia. J Alzheimers Dis 50:1217-1225. [Crossref]
- Van Kooten J (2019) Samenvatting proefschrift. Pijn bij mensen met dementie, met speciale aandacht voor verpleeghuis bewoners. NTvGF 4.
- J Mc Kay, L Ting (2020) Perception of whole body motion during balance perturbations is impaired in Parkinson disease and is associated with balance impairment. Gait Posture 76: 44-50. [Crossref]
- Kraft P, Gadeholt O, Wieser M, et al. (2009) Lying obliquely-a clinical sign of cognitive impairment: cross sectional observational study BMJ 339: b5273. [Crossref]
- Karnath HO. (2000) The origin of contraversive pushing. Neurology 1: 1298-1304.
- Karnath HO, Baier B (2010) Right insula for our sense of limb ownership and self-awareness of actions. Brain Struct Funct 214: 411-417. [Crossref]
- Robinovitch S, Feldman F, Yang Y, et al. (2012) Video capture of the circumstances of falls elderly people residing in long -term care: an observational study. Lancet.
- Duysens J (2015) Differences in foot sensitivity and plantar pressure between healthy young and elderly. Arch Gerontol Geriatr 63: 67-71. [Crossref]
- Kool J (1992) Seriengipse zur kontrakturbehandlung in der neurologische rehabilitation. Der Physiotherapeut 2: 14-21.
- Goldspink G, Tabary C, Tabary JC, (1974) Effect of denervation on the adaptation of sarcomere number and muscle extensibility to the functional length of the muscle. J Physiol 236: 733-742. [Crossref]
- Bautmans I, Demarteau J, Cruts B, et al. (2008) Dysphagia in elderly nursing home residents with severe cognitive impairment can be attenuated by cervical spine mobilisation. J Rehabil Med 40: 755-760. [Crossref]
- Tieland M (2019) Sarcopenie, etiologie en interventies. Physios.
- Van de Rakt (2019) Transfers book: the skills of the resident in an Nursing home as the base for therapeutic and Movement Guiding Care. Scholars Press.
- Bosch F (2010) Krachttraining en coördinatie. Uitgevers.
- Hettinger T (1983) Isometrisches Muskeltraining. Thieme Verlag Stuttgart.
- Van de Rakt J (2001) Het Rakt concept. Tijdschrift Fysiotherapie en Ouderenzorg 2: 22-33.
- Van de Rakt J, Mc Carthy Grunwald S (2020) Physical treatment of individuals with dementia. Part 1 A. Ita J Sports Reh Po 2: 1546 -1581.
- Realiteit Orientatie training (ROT). [Crossref]
- Feil N (1982) Validation, Versluys.
- Warm care (btsg.nl/warme-zorg).
- Van Puyenbroek J Maes B (2008) A Review of Critical, Person‒centred and Clinical Approaches to Reminiscence Work for People with Intellectual Disabilities. INT J DISABIL DEV ED 55.
- Baart A (2004) Een theorie van de presentie. Uitgevers: Boom Lemma.
- Brooker D (2005) Dementia Care Mapping. A Review of the Research Literature. The gerontologist 45: 11-18. [Crossref]
- Van Eijle J (1995) Wie wat waar? in PDL. SMD. Educatieve Uitgevers.
- M Graff (2010) The EDOMAH-approach Thesis.
- Barbossa R, Silva N, Santoas D, et al. (2020) Force stability training decreased force variability of plantar flexor muscles without reducing postural sway in female older adults. Gait Posture. [Crossref]
- Van de Rakt j, Mc Carthy Grunwald S (2015) Diagonals: Part One. Ita J Sports Reh Po.
- Van de Rakt J, McCarthy Grunwald S (2015) Diagonals part 2-Assessment and Trunk Rules. Ita J Sports Reh P.
- Van de Rakt J, McCarthy Grunwald S (2018) Diagonals Part 7 Stroke 5 Walking: What say the scientist and what is best practice. Ita J Sports Reh Po 2: 1013-1062.
- Van de Rakt J, McCarthy Grunwald S (2019) Diagonals Part 8 Stroke 6 analysis of walking pattern and treatment. Ita J Sports Reh Po 2: 1191-1238.
- Van de Rakt J, McCarthy Grunwald S (2015) Diagonals Part 9 Analysis of walking pattern. Learn to assess. Ita J Sports Reh Po 2: 1253-1294.
- Blair A, Manian F (2017) Coexisting Systemic Infections in Patients Who Present With a Fall. Am J Med Sci 353: 22-26. [Crossref]
- Leeuwis A, Kuiper A, Schreuder C, et al. (2019) Ondersteuning bij visuele problemen in het kader van posterieure corticale atrofie-een casus. Neuropraxis.
- James M, Plant G, Warrington E (2001) Cortical Vision Screening Test: Manual&Test Materials Unknown Binding.
- Riemersma van der Lek RF, Swaab DF, Twisk J, et al. (2008) Effect of bright light and melatonin on cognitive and non-cognitive function in elderly residents of group care facilities: a randomized controlled trial. JAMA.
- Zwakhalen S (2016) Herkenning en behandeling van pijn bij kwetsbare ouderen. Verenso.11-88.
- Neumann DA (1999) Proefpersonen met een heupoperatie die op verschillende manieren lopen met een stok. Stimulus 4: 387-394.
- Peeters L, Janssen M, Kingma I, et al. (2016) Compensatory trunk movements during functional tasks in patients with Duchenne muscular dystrophy. Arq Neuropsiquiatr 72: 5-11. [Crossref]
- Lundin Ollson L (1997) Stops Walking when talking as a predictor of falls in elderly people. Case report. The Lancet 349.
- Norton K, Norton L, Sadgrove D (2010) Position statement on physical activity and exercise intensity terminology. J Sci Med Sport 13: 496-502. [Crossref]
- Sinnige Orij P, Lagaay A (2006) Wat zijn de effecten van algemene narcose op de cognitieve functies op hoge leeftijd? Vademecum permanente nascholing huisartsen.
- Alıci N, Zorba Bahceli P, Nuran Emiroğlu O (2018) The preliminary effects of laughter therapy on loneliness and death anxiety among older adults living in nursing homes: A non randomised pilot study. Int J Older People Nurs. [Crossref]
- Bertens D, Fasotti L, Boelen D, et al. (2013) A randomized controlled trial on errorless learning in goal management training: study rationale and protocol. BMC Neurology 13: 64.[Crossref]
- Robinovitch S (2016) Risk factors for hip impact during real life falls captured on video in long term care. Osteoporos Int. [Crossref]
- Pijnappels M (2005)Vallen bij ouderen. Stimulus.
- Bear M, Connors B, Paradiso M (2001) Neuroscience library of congress.
- Kaas J (1999) The reorganisation of sensory and motor maps after injury in adult mammals. J Cogn Neurosci 45-63.
- Recanzone GH (1999) Cerebral cortical plasticity: perception and skill acquisition The J Cogn Neurosci 16: 133-156. [Crossref]
- Beek (2010) Motorisch leren Sportgericht 1-10.
- Henz D, Schollhorn W (2016) Differential training Facilitates Early consolidation in Motor learning. Front Behav Neurosci 10:199. [Crossref]
- Fedor A (2015) The Effects of A Brief, Water-Based Exercise Intervention on Cognitive Function in Older Adults. Arch Clin Neuropsychol 30: 139-47. [Crossref]
- Voncken en anderen, BrabantZorg (2014) Pilot: Bewegen met water. Team Bewegingsagogie en Psychomotorische therapie. NHV nieuwsbrief 4. [Crossref]
- Sato M, Miyake J, Hashimoto Y, (2010) Tactile Perception of a Water Surface: Contributions of Surface Tension and Skin Hair.
- Sato D, Onishi H, Yamashiro K, et al. (2011) Water Immersion to the Femur Level Affects Cerebral Cortical Activity in Humans: Functional Near-Infrared Spectroscopy Study. Brain Topography 25: 220-227. [Crossref]
- Sato D, Yamashiro K, Onishi H, et al. (2012) The effect of water immersion on short-latency somatosensory evoked potentials in human. BMC Neuroscience.
- Van de Rakt J, Mc Carthy Grunwald S (2022) Physical treatment (Hydrotherapy) by individuals with and without dementia. Aquatic exercising. Part 1 Ita J Sports Reh Po 3: 1989-2017.
- Van de Rakt J, Lambeck J (2004) Therapeutisch zwemmen met" verpleeghuis" patiënten? N.V.F.G.
- Myers K, Capek D, Shill H, et al. (2013) Aquatic Therapy and Alzheimer ’s disease Annals of Long-Term Care: Clinical Care and Aging.
- Bautmans I, Demarteau J, Cruts B, et al. (2008) Dysphagia in elderly nursing home residents with severe cognitive impairment can be attenuated by cervical spine mobilisation. J Rehabil Med 40: 755-760. [Crossref]
- Burnfield J, Shu Y, Buster T, et al. (2012) Kinematic and electromyographic analyses of normal and device-assisted sit-to-stand transfers. Gait and Posture. [Crossref]
- Van de Rakt J, Mc Carthy Grunwald S (2020) Treatment possibilities of “contractures “by neurological diseases. Ita J Sports Reh Po 7: 1450 -1478.
- Van de Rakt J, McCarthy Grunwald S (2016) The beginning of ‘striker foot’ (Pes equinus varus) with severe stroke patients. Ita J Sports Reh Po 1: 476-497.
- Leonie Bruil, Marian J, M Adriaansen, et al. (2017) Kwaliteit van leven van verpleeghuisbewoners met dementie voor, tijdens en na het spelen met de Tovertafel. Tijdschr Gerontol Geriatr. Kwaliteit van leven van verpleeghuisbewoners met dementie voor, tijdens en na het spelen met de Tovertafel 36: 516-22. [Crossref]
- Butler DS (2000) The sensitive nervous system. Noigroup Publication.
- Shack locks M (2005) Clinical Neurodynamics. Elsevier, Butterwoth, Heinemann.
- Butler S (1991) Mobilisation of the nervous System. Churchill Livingstone.
- Staarink, HAM. (2014) Zo zit het. Koninklijke van Gorkum BV, Assen.
- Engstrom B (2003) Ergonomie sitzen im rollstuhl.
- Engstrom B (2002) Ergomic seating an true challenge.
- Schellebach J, Werkhoven N, Vd Rakt J (2005) Invloed van het 2 uur zitten in een rolstoel met een slappe zitting op het alignment van het aangedane been, het aantal stappen en de snelheid van het gaan bij een CVA-patiënt. Keypoint.
- Van de Rakt J, Mc Carthy Grunwald S (2021) Swallowing and the attitude of the neck/body. Ita J Sports Reh Po 8: 1745-1783.
- Heytens S (2011) Diagnose van het lumbaal spinale-stenose-syndroom.Vakgroep Huisartsgeneeskunde en Eerstelijnsgezondheidszorg, Universiteit Gent. Minerva mei volume 10 nummer 4.
- Cyriax J (1982) Textbook of orthopaedic medicine. Volume one. Bailliere Tindall London.
- Cyriax J (1984) Texbook of orthopaedic medicine. Bailliere Tindall London.
- Burnnstromm S (1970) Movement therapy in hemiplegia. Harper&Row.
- Vd Rakt J (2018) The environment in long-care facilities (Nursing home) decrease the possibilities to move independent! GJRA 12: 2-10.
- Cools L (2007) Bewegen en bewogen worden PAOG uitgave Nijmegen.
- Vd Rakt J (1997) Hypothese over het ontstaan van de foetale houding. Tijdschrift voor Fysiotherapie en ouderzorg 15: 25-29.
- Bohannon R, Suith M (1987) Interrater reliability of a modified Ashworth scale of muscle spasticity Phys.Ther 67: 206-207. [Crossref]
- Collin C, Wade D (1990) Assessing motor impairment after stroke: a pilot reliability study. J Neurol Neurosurg Psychiatry 53: 576-579. [Crossref]
- Waardenburg H, en anderen (1999) Is paratonie betrouwbaar te meten ? Ned.Tijdsch v Fysio nummer 2.
- Husain T (1953) Pressure sores. J Path Baet 347.
- Van de Rakt J, Mc Carthy Grunwald S (2021) Rehabilitation of the upper limb after an stroke. Part 1. The Flexion Attitude Synergy. An multi-eclectic approach. Ita J Sports Reh. Po 8: 1829-1867.
- Middelveld I (1986) Paratonie Ned. Tijdschrift voor fysiotherapie 4.
- Arnts H (1989) Paratonie en de fysiotherapeutische behandeling. Ned.Tijdschrift voor Fysiotherapie 7: 9.
- Vallar G, Rusconi M, Bignamin L, et al. (1994) Anatomical correlates of visual and tactile extinction in humans. J Neurol Neurosurg Psychiatry 57: 464–470. [Crossref]
- Branten J, Wasenberg I (2003) Bestrijding van contracturen bij chronische neurologische patiënten d.m.v het corrigeren van de rusthouding. Vakblad NVFG.
- Van de Rakt J (2001) Stinkende handen . Keypoint 1.
- Law C (2019) Physical exercise attenuates cognitive decline and reduces behavioral problems in people with cognitive impairment and dementia: a systematic reviewJ PHYSIOTHER 66: 9-18.