Skin microbiome is a network of bacteria, fungal, viral, and parasitic organisms that reside on the skin and are significant for skin health and disease. This review aims to contribute to a discussion of how skin microbiota modulates or is modulated by several ailments associated with skin, including viral warts, molluscum contagiosum, psoriasis, and chronic dermatitis. The data reveal the consequences of changes in the composition of the intestinal microbiota and its disorders, which are examined to determine the state of the microbiome in these diseases. Hence, the review then discusses new research findings that ascertain the microbiome to be implicated in disease skin development and relapse and the possibilities of using microbiome-oriented therapy. Therefore, dissection of these microbial interactions effuses possibilities for subsequent treatment and prevention measures against skin disorders to boost dermatological intervention. It can provide useful data on the subject, such as what the inhabitants of the skin microbiota do, and it can be used for diagnostics or treatment of diseases.
Dermatological Disorders; Skin Layer; Skin Microbiome; Health
The outer skin layer, which is also the largest, is the external cover of the human body and is populated by countless microorganisms, as well as microscopic bacteria, fungi, viruses, and tiny mites. As a whole, this population-dense group, referred to as the skin microbiome, comprises an essential defense system against pathogens and the regulation of immune functions, as well as the skin's mechanical integrity. It has been noted that skin microbiota plays a crucial role in attaining skin homeostasis, and its imbalance proves to be a factor in several skin disorders. Recent carriers deeply describe the role of microbiota in skin life and its potential impact on physiology and pathology. It is critical to comprehend how the host's properties influence the interactions between the skin's microbiome and pathogenic microorganisms, as well as commensal organisms, in order to create new antifungal approaches that will help restore the skin microbiota balance and treat skin diseases. This review aims to describe these relatively dynamic interactions and how each of the factors presents in usual dermatological diseases.
The Skin Microbiome's Role in Dermatological Health
This project offers fresh evidence that instead of being mere tenants of skin, microbes are also stakeholders who play an active role in skin affairs. It does significantly differ amongst the different sites of the human body depending on factors such as the environmental conditions, cleanliness of the human host, and overall health status [1, 2]. This microbial community serves multiple critical functions: it builds a barrier against invading pathogens, generates necessary nutrients, and acts as a training ground for immunological response to microbial antigens. Balancing this microbiota is equally important for controlling infections and preserving the healthy status of the skin. Disturbances in the skin microbiota of organisms termed dysbiosis have been demonstrated to predispose the body to infections, worsen conditions like psoriasis, and even shift immune responses in the body. This review discusses the critical aspect of trying to keep the relative balance of skin microbiota and reveals possible implications of balance disruption while highlighting the possibilities of microbiota manipulation targeting skin diseases.
Viral Warts and the Microbiome
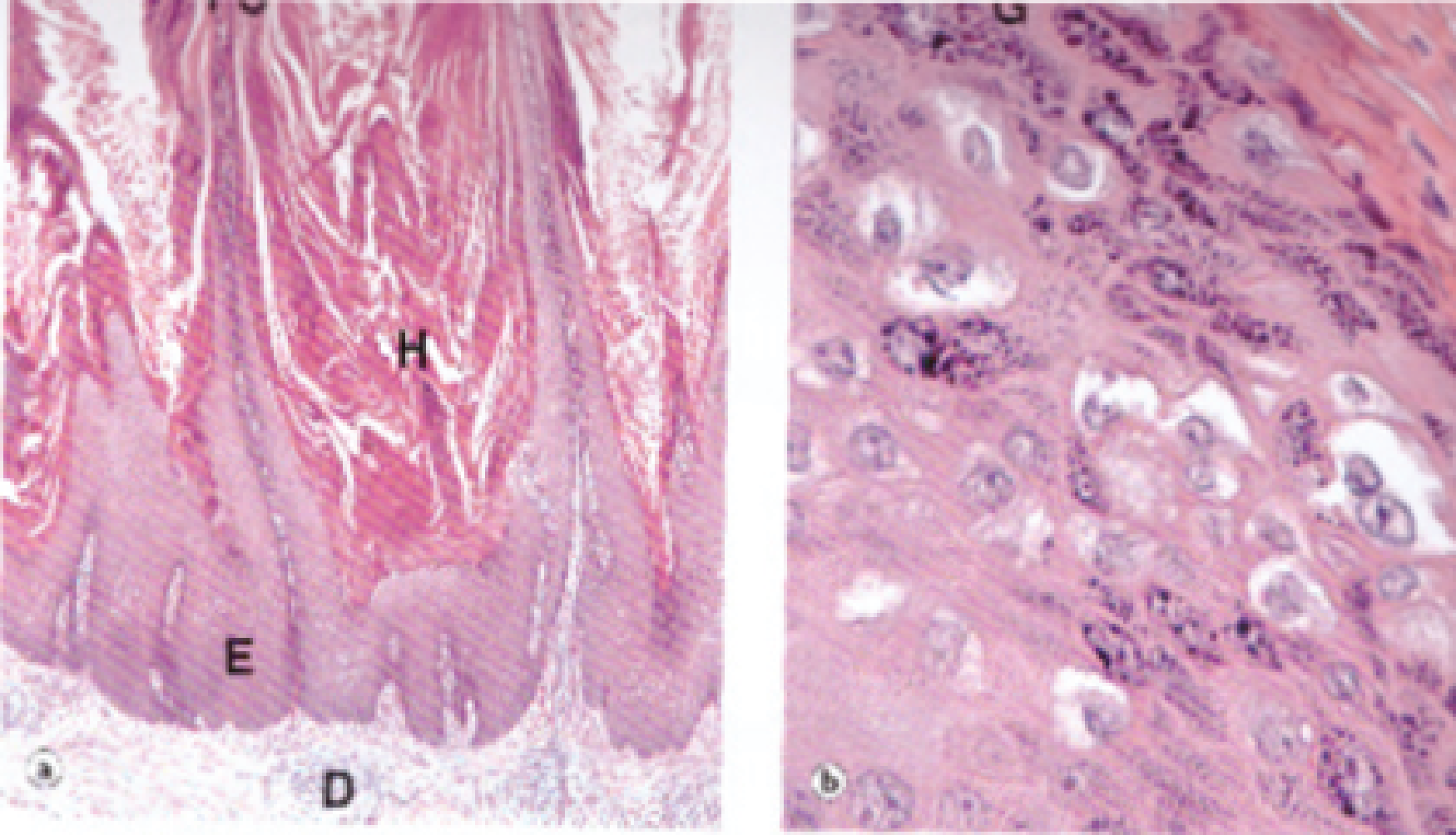
Some of the communal planes include planes such as papillomavirus, which is a human complication that is papillomatous, affecting both skin and mucous membranes, and many HPV strains are likely to cause the infections. Another complicated interaction is the one between HPV and skin biofilm, as the microbial consortia can either weaken the virus's ability to colonize and persist on the skin or increase its pathogenicity [3, 4]. In the existing literature, it is mentioned that an appropriate and effective combination and diversity of microbiota is positive for HPV since bacteria replace antibodies and compete with the virus for required sites and nutrients, as well as regulate the immunity of tissues. In contrast, a disrupted microbiome may prevent the return of normal microbiota that would otherwise inhibit the growth of viral warts by consuming the nutrients and, thus, improving the nutrition of the virus, which will enable it to continue to exist; therefore, there's the likelihood of using microbiome to enhance treatment and prevention interventions.
Molluscum Contagiosum and Microbial Interactions
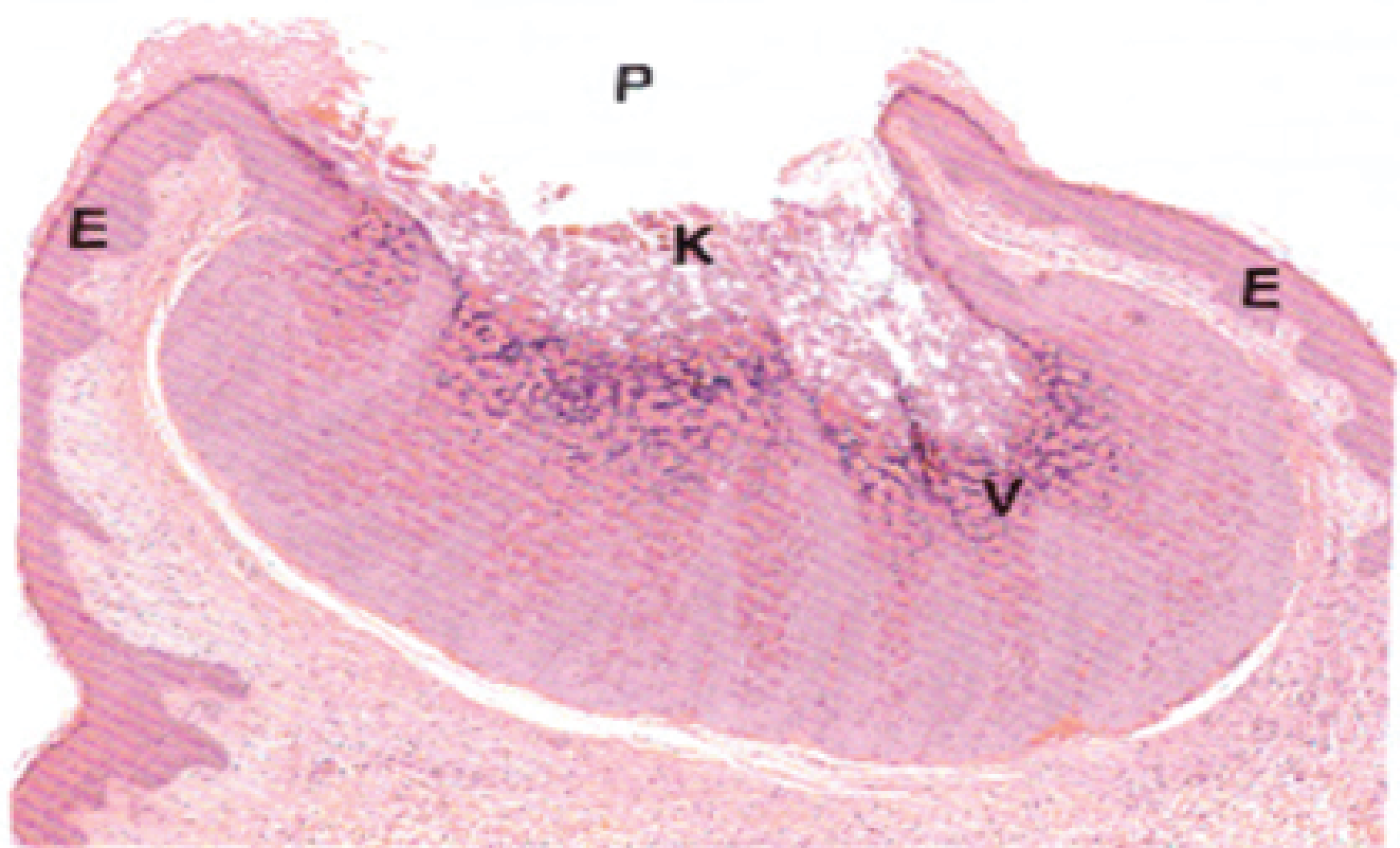
Molluscum contagiosum, which is a pox virus disease, presents with small umbilical papules with shining centers usually localized in children and immunocompromised persons. With reference to this viral infection, the focus has been made to establish a link between the skin microbiome and the progression and regression of this illness [3]. The location of the skin microbiome hub impacts the viral life cycle and the host's immune responses. All of this influences the distribution and clearance of skin lesions. Interference with skin microbiota can lead to an increase in the virus because skin integrity would be disrupted and immune defense decreased; at the same time, the skin microorganisms can regulate the viral infection by inhibiting it and promoting immunity effectively at the skin level. This would give information about potential bacteriophage-based therapies targeting the microbiome.
Psoriasis and the Microbiome
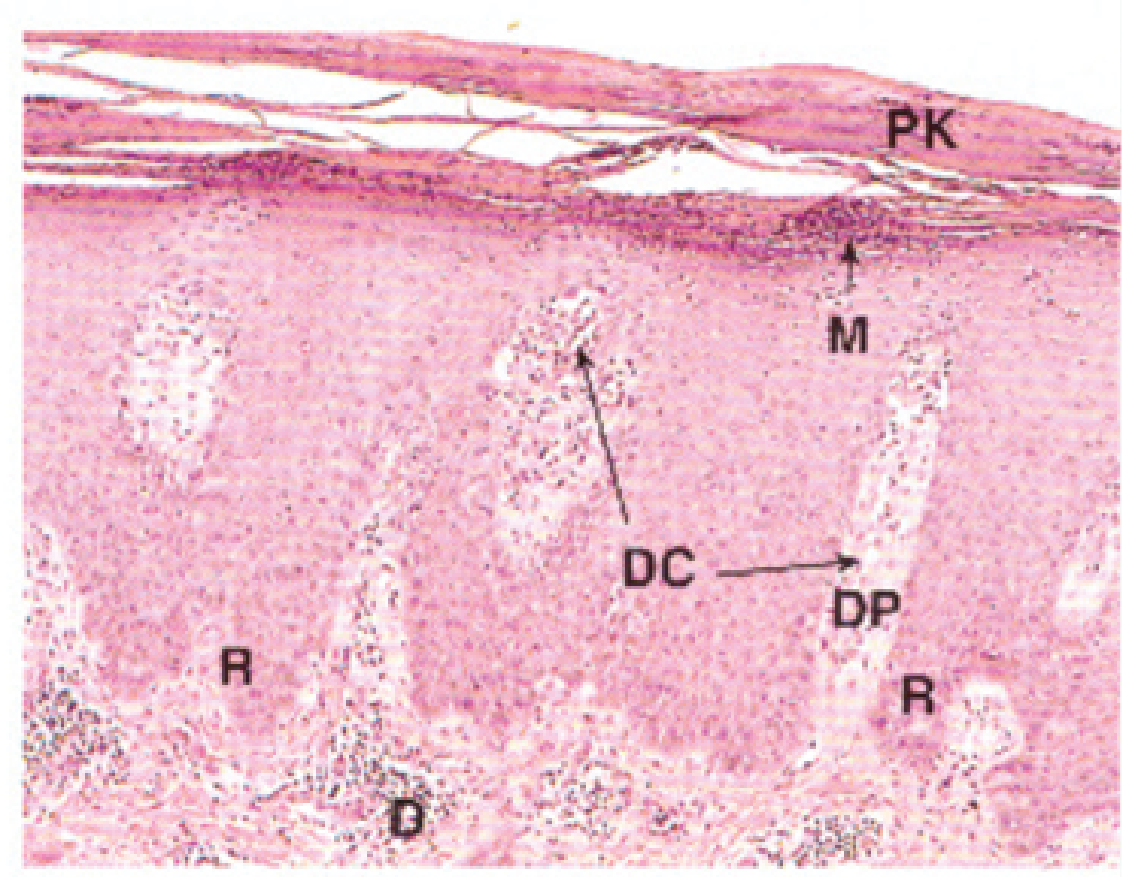
Psoriasis is an autoimmune skin disorder that is characterized by red patches that are either smooth or elevated and are covered by a silvery white or grey sheen. This condition is primarily dermatologic, though it can present mucocutaneous and systemic manifestations occurring in joints and other organs. Other microbial imbalances were observed in psoriatic lesions, such as a shift in the microbial profile, which could act as a stimulus for inflammation in psoriasis. In particular, they observed diminished skin microbial population density and increased abundance of portend pathologic bacterial groups, including Streptococcus and Staphylococcus species. It is also known that these microbial changes are directly implicated in the inflammatory processes associated with this skin disease. In addition to this [1], also reported a correlation between the shift in skin microbiota and the factors relating to the clinical activity of the disease, thereby propounding the aspect of microbial dysbiosis as a potential triggering factor for the range of manifestations of psoriasis.
Chronic Dermatitis and the Microbiome
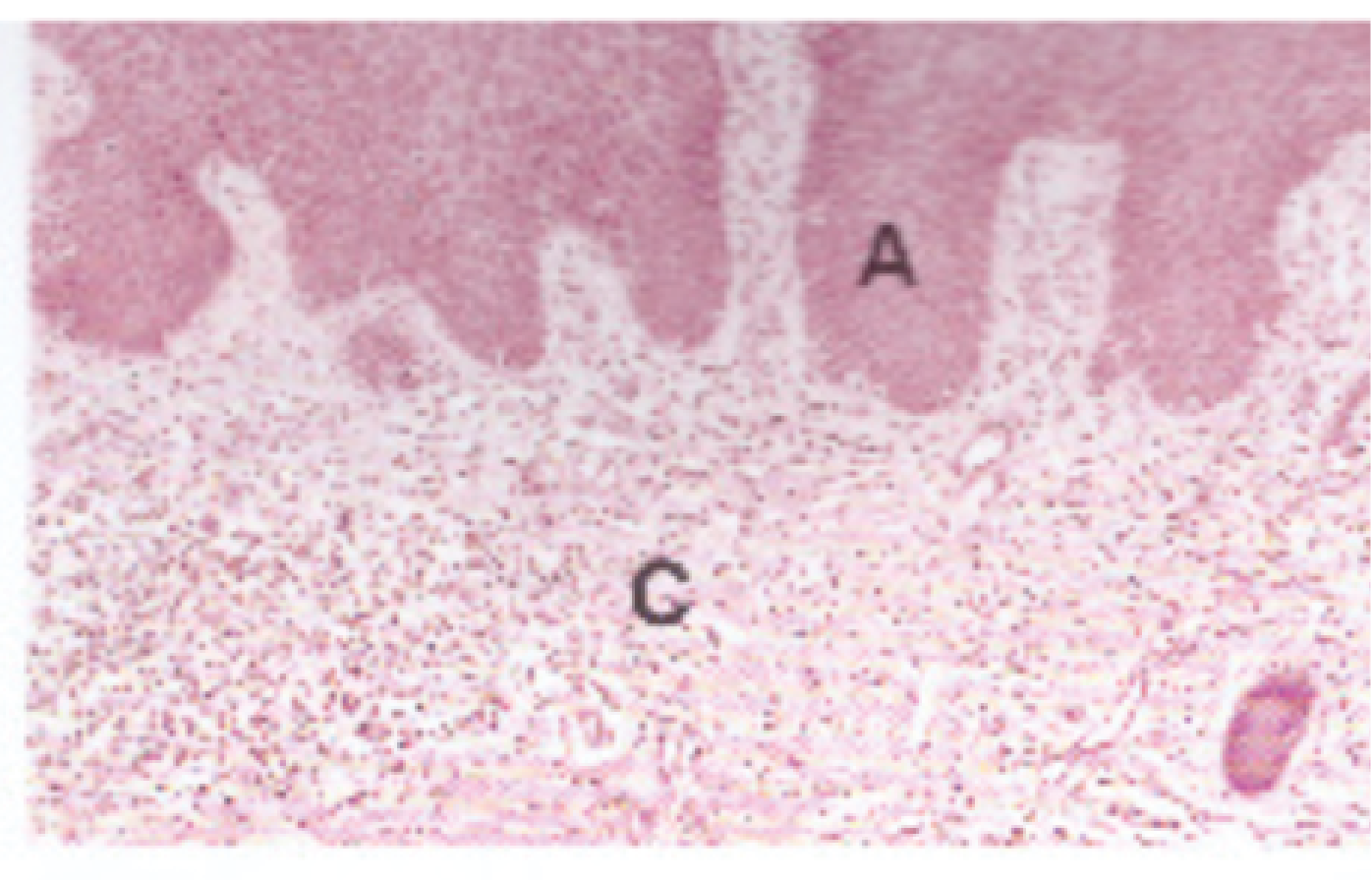
Signs related to chronic dermatitis, such as atopic dermatitis, are typical skin complaint types with a solid ability to regard typical and unhealthy microbial congregation. It is established that infants and young children with this condition usually display increased colonization with staphylococcus aureus, a bacterium known to cause the worsening of atopic dermatitis and increase the severity of the disease. Excessive growth of any of these microorganisms may destroy the average point yield of skin microflora, increase immune response and deteriorate the already impaired barrier function of the skin.
Science proves that adjustments in selection by the critical microbe might open different treatment solutions for chronic dermatitis. It is possible to deploy such alterations in the microbial orchestra of skin to decrease inflammation, heal disrupted skin barriers and enhance skin health in general. They may include the administration of certain organisms that would help to increase the production of beneficial bacteria and decrease bad ones or feedstocks meant for such bacteria. The discussed prospect of microbial intervention underlines that emerging knowledge of bacterial-skin immune pairings is essential in chronic dermatitis etiology and treatment [3, 4].
Skin microbiota has emerged relatively recently as a potential major contributor to dermatological diseases, and its investigation is still dynamically progressing, thus offering potentially significant breakthroughs with regard to these states. The importance of microbial balance in skin care continues to manifest as research advances – establishing the need to adopt balanced microbial skincare to solve skin health problems. More research is required to give a better understanding of how the skin microbiome and immune system work together to execute their functions, with the objective of developing a new therapeutic approach using the skin microbiome.
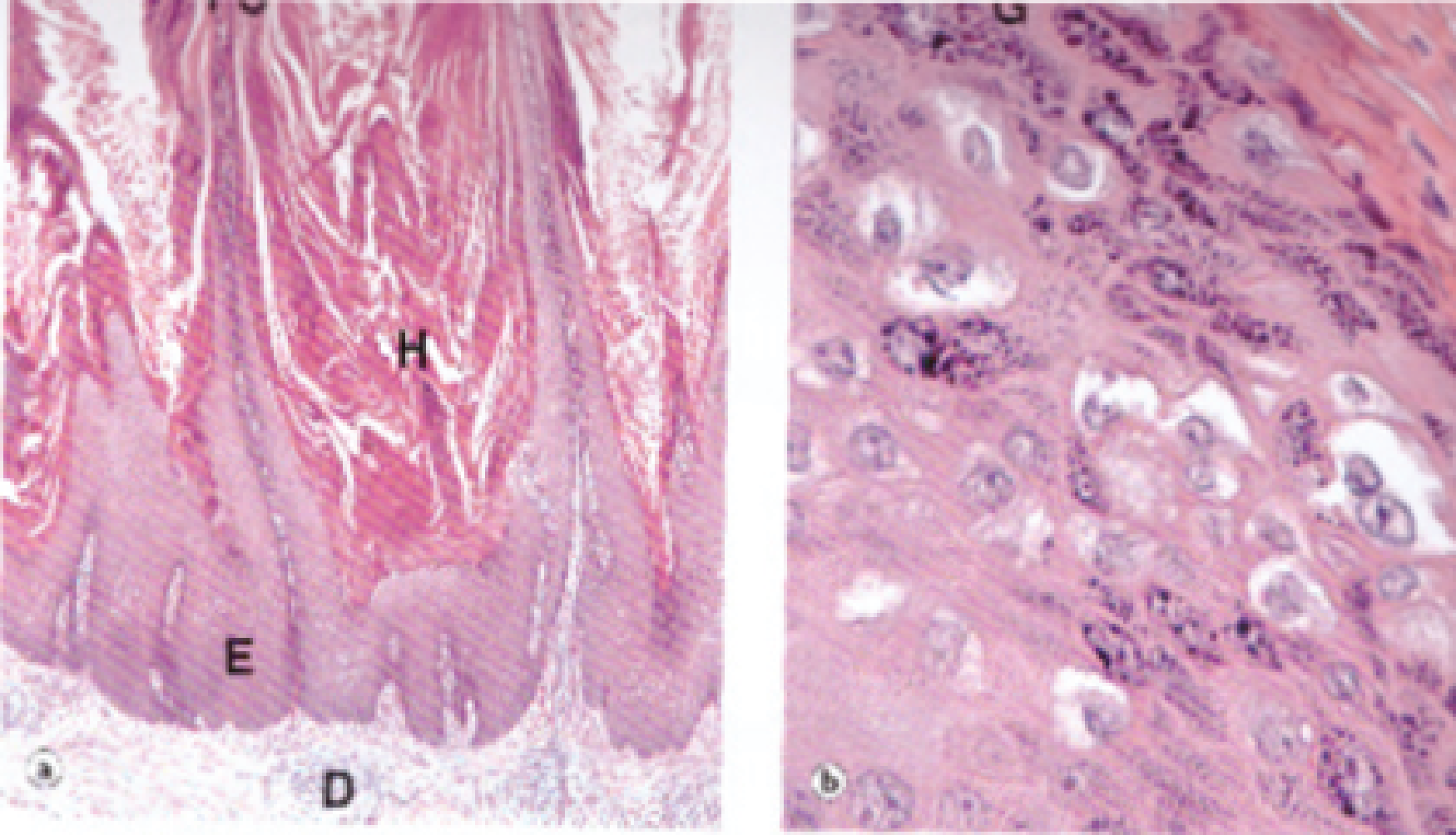
Figure 1: Viral Warts
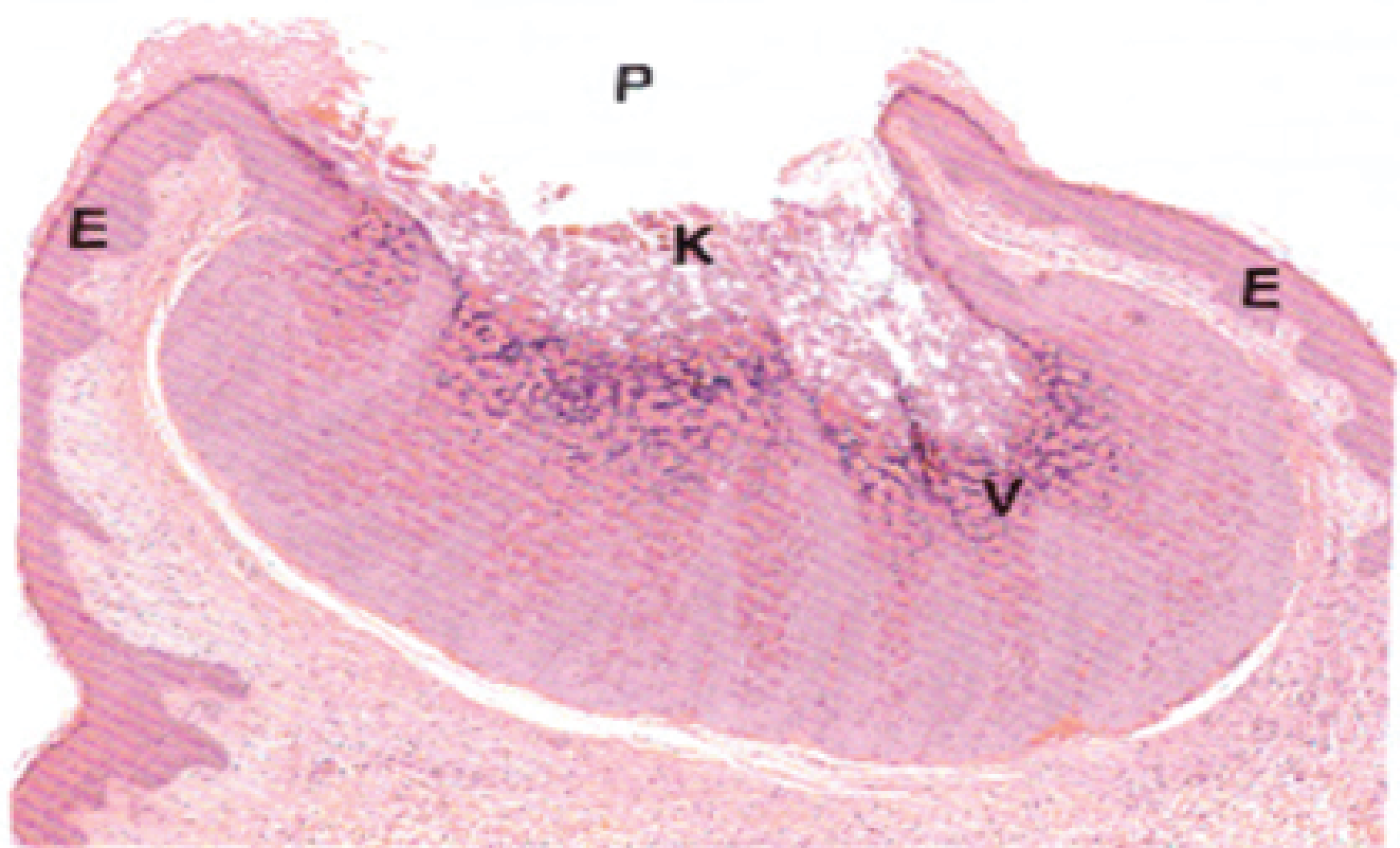
Figure 2: Molluscum Contagiosum
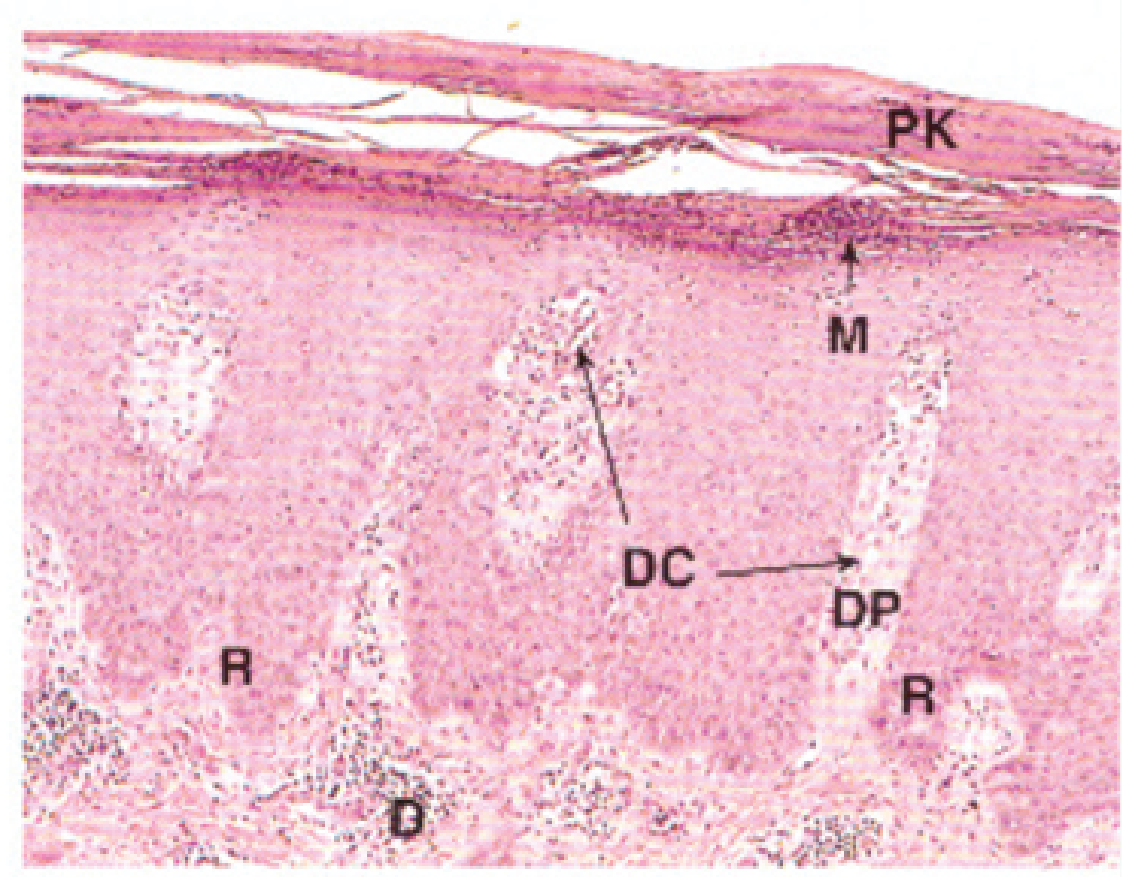
Figure 3: Psoriasis
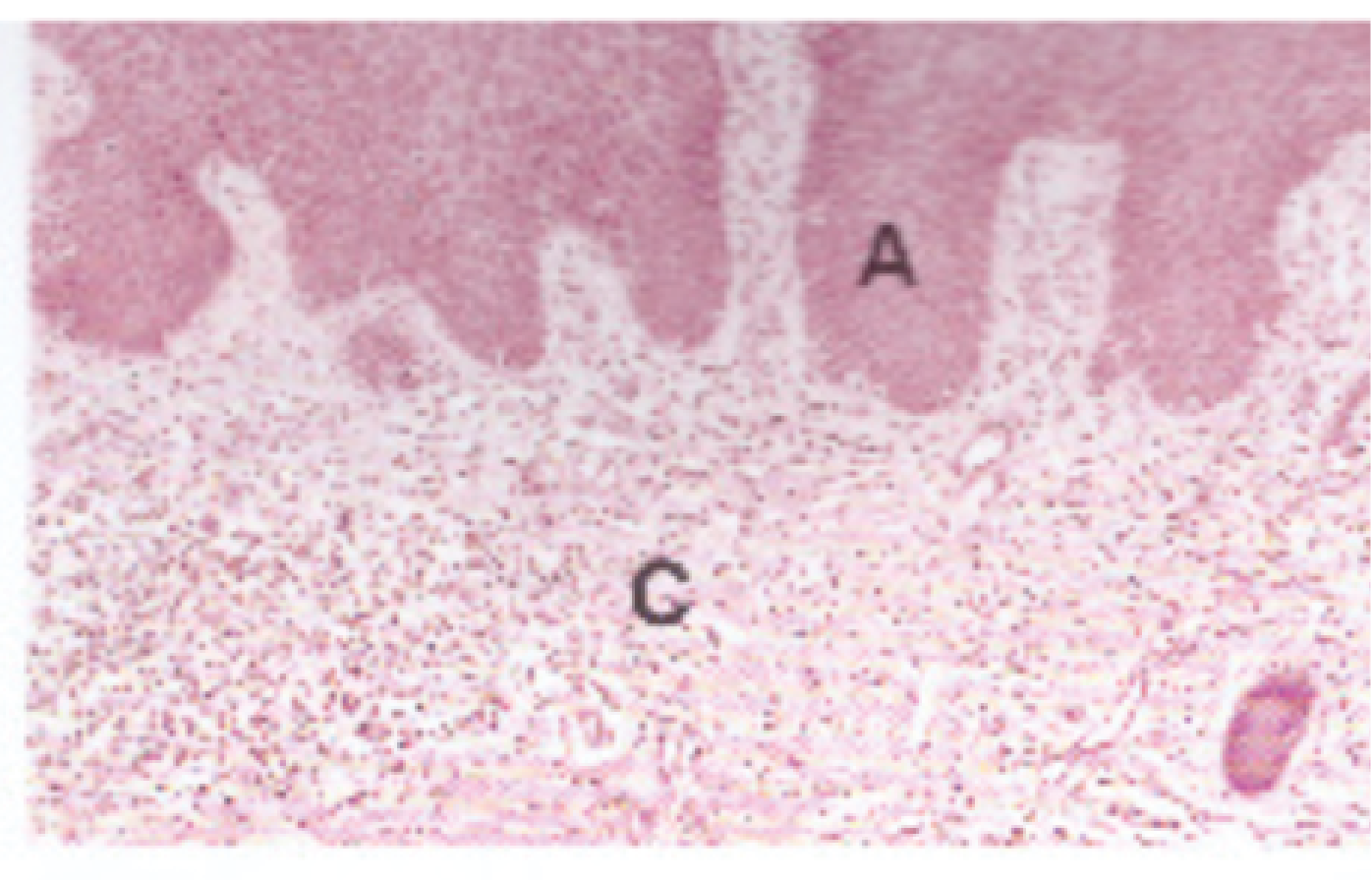
Figure 4: Chronic Dermatitis
- Edwards, A., Cameron, K. A., Cook, J. M., Debbonaire, A. R., Furness, E., et al. (2020) Microbial genomics amidst the Arctic crisis. Microbial Genomics 6. [Crossref]
- Han, J. H., Kim, H. S (2024) Skin deep: The potential of microbiome cosmetics. Journal of Microbiology 1-19. [Crossref]
- Slater, A., Nair, N., Suétt, R., Mac Donnchadha, R., Bamford, C., et al. (2022) Visualising Viruses. Journal of General Virology, 103(001730). [Crossref]
- Whiting, C., Abdel Azim, S., Friedman, A (2024) The Skin Microbiome and its Significance for Dermatologists. American Journal of Clinical Dermatology 1-9. [Crossref]