Background: While the medical fee system for acute care in Japan provides incentives to ensure that patients are discharged early, it does not incentivize the direct reduction of postoperative complications. This retrospective study highlighted the importance of rewards for providing high-quality surgery to patients requiring open colectomy to reduce postoperative complications. The impact of postoperative complications on hospital stay length was investigated.
Methods: This study analysed 1,096 patients who underwent open colectomy between May 2004 and December 2008. A stepwise multiple regression analysis was performed to estimate the effect of complications on the length of hospital stay. The Kaplan–Meier survival analysis was used to estimate the cumulative probability of hospital stay.
Results: The mean length of hospital stay was 24.84 (SD=2.25) days. Approximately 0.9% of the patients experienced postoperative peritonitis, while 2.5% experienced postoperative ileus. The hospital stay length was prolonged by 69.9% and 51.6% (p<0.01) for the patients with postoperative peritonitis and postoperative ileus, respectively. The cumulative probability was higher for patients with complications than those without complications.
Conclusion: This study provides empirical evidence on the need to improve the quality of surgery, which will benefit patients and hospitals. It also highlights the importance of providing additional rewards to reduce postoperative complications.
Open Colectomy; Postoperative Peritonitis; Postoperative Ileus; DPC/PDPS
In Japan, the medical fee system for acute care is guided by the Diagnosis Procedure Combination/Per Diem Payment System (DPC/PDPS). The rationale behind this system is that hospitals provide acute care to patients with a high awareness of the management of the length of their stay (LOS). This is in addition to providing a clinical diagnosis and medical treatment.
However, highly invasive surgeries, such as open colectomy, are often associated with complications; therefore, the LOS is prolonged. The incidence rate of postoperative complications after an open colectomy was reported to be 27.3% in a sample of n=1,657 [1]. The main complications following an open colectomy are postoperative peritonitis -which is caused by surgical site infection and anastomotic leakage-and postoperative ileus-which can result from intestinal dyskinesia due to intestinal paralysis or dilation through open surgery [2-6]. These complications are associated with either intra-abdominal adhesions or inadequate anastomosis techniques [3-6]. As for postoperative ileus, a previous study reported that the incidence of postoperative ileus prolonged the LOS by 29% [6]. Most studies did not show the cumulative probability of hospital stay, while they estimated the probability of survival due to complications.
The DPC/PDPS is not designed to provide direct incentives to acute care hospitals and reduce the incidence of postoperative complications related to colorectal cancer. This system is merely a mechanism that indirectly improves the quality of acute care by providing incentives to ensure that the patients are discharged early.
Reducing the risk of postoperative complications requires designing a framework to improve a surgeon’s surgical technique. Accordingly, hospitals will actively improve the quality of medical care if the surgical techniques that improve patient prognosis can be properly evaluated. This retrospective study highlights the importance of additional rewards for performing high-quality surgery on patients requiring open colectomy to reduce postoperative complications. The effects of postoperative peritonitis and postoperative ileus on the patients’ LOS were analysed.
Study Design and Patients
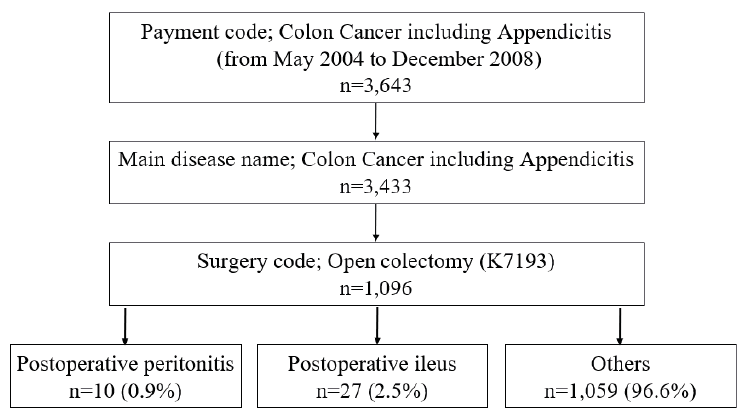
This study analysed the medical claims of 3,643 patients diagnosed with malignant tumours in the colon in 24 hospitals in Japan (Figure 1).
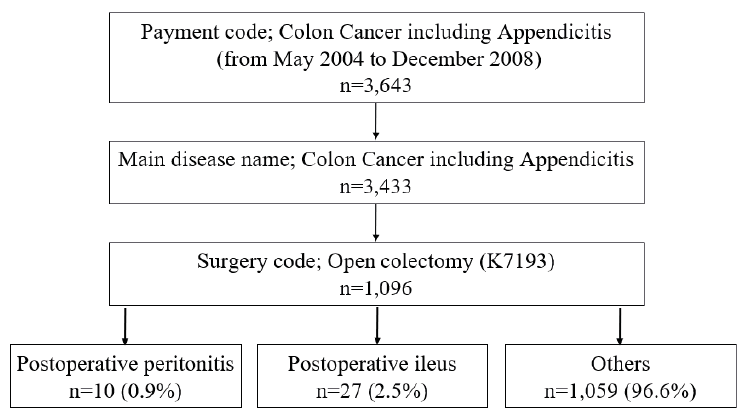
Figure 1: Flow chart of data extraction
Among them, 1,096 patients (male: n=601, female: n=495) had undergone an open colectomy-verified by checking their medical records. According to the medical fee code, open colectomy is classified as a major diagnostic category for a malignant tumour of the colon. The data contained outcomes ranging from ‘complete recovery’ to ‘death of the patients’. The data collection period ranged from May 2004 to December 2008. This period corresponded to the initial stage of DPC/PDPS enforcement. Thus, it covered the medical treatment provided under the new national medical service fee system at the time. Therefore, the changes in the system may have had some impact on patients’ LOS. Although the data is old, the diagnostic criteria of patients requiring surgery for an open colectomy remain fundamentally unchanged [7, 8]. This study was approved by the Ethics Review Board in the International University of Health and Welfare, Japan.
The distributions of patients’ ages and LOS were analysed using the Kolmogorov–Smirnov test. They were divided into ‘positive’ and ‘negative’ groups with and without complications for both variables: postoperative peritonitis and postoperative ileus. When equal variance could not be assumed, pairwise comparisons of the means of the groups were conducted using Welch’s t-test. Levene’s test was used when appropriate.
A stepwise multiple regression analysis was performed with the two complications, postoperative peritonitis and postoperative ileus, to estimate their effect on the LOS. Additional treatments (central intravenous injection, radiotherapy, and chemotherapy), defined in the DPC/PDPS as medical fee codes, were included as dummy variables. Regarding their age, the patients who were 80 years or older were included as dummy variables because such patients with colectomy have a relatively high risk of postoperative complications [9]. In addition, gender factors were included as dummy variables because male patients have a relatively higher risk of postoperative complications [1, 3]. Regarding the severity level, the pathologic stage was weighted as a dummy variable because it is necessary to observe the impact of patient factors on the LOS within the constraints of the data. The formula used for the estimation was:
lnDi=α+β1A+β2M+β3S1+β4S2+β5S3+β6S4+β7PP+β8PI+β9CI+β10RT+β11CT+εi.
The independent variable Di denotes the LOS (natural logarithm). The dependent variables included are as follows: A, a dummy variable observing whether the patient was aged 80 or above. M, a dummy variable observing whether the patient was a male or female. S1, S2, S3, and S4 are dummy variables observing whether the patient had a pathologic stage I, II, III, or IV tumour, respectively. PP is a dummy variable observing whether the patient had postoperative peritonitis. PI is a dummy variable observing whether the patient had postoperative ileus. CI is a dummy variable observing whether the patient received the central intravenous injection. RT is a dummy variable observing whether the patient underwent radiotherapy. CT is a dummy variable observing whether the patient underwent chemotherapy, and εi is the error term. Each dummy variable is set to one if the independent variable is applicable. No multicollinearity was observed in the data.
The Kaplan–Meier survival analysis was used to estimate the cumulative probability of hospital stay for each group of patients irrespective of whether they exhibited complications. Pairwise comparisons of the positive and negative groups of patients with and without complications among the variables were conducted using the log-rank test. The event for starting to follow a patient indicates the probability of discharging from acute hospitals or their acute care beds.
a After conducting the stepwise multiple regression analysis, a power analysis was performed.a IBM SPSS 26.0 J for Windows was used to conduct the analyses.
Table 1 shows the patients’ descriptive statistics. Although open colectomy is associated with a high risk of complications due to its invasive nature, only 337 patients showed a high severity of illness (pathologic stage III, 21.1%; stage IV, 9.7%). Furthermore, only 66 patients underwent additional treatment through central intravenous injection (3.2%), radiotherapy (2.6%), and chemotherapy (0.2%). The LOS average increased with age. The mean and standard deviation of the LOS is 24.84 ± 12.25.
Table 1: Descriptive statistics of the patients
Number of patients |
1,096 |
≥80 years |
205 (18.7%) |
Age (Mean ± SD) |
69.54 ± 11.62 |
Age (Range, Q1, Q3) |
21–96, 63, 77 |
Male: Female ratio (n, %) |
601:495 (54.8%:45.2%) |
Pathologic stage (n = 1,096) |
|
Stage 0 (n, %) |
21 (1.9%) |
Stage I |
123 (11.2%) |
Stage II |
210 (19.2%) |
Stage III |
231 (21.1%) |
Stage IV |
106 (9.7%) |
Not indicated |
405 (37.0%) |
Outcome (n = 1,096) |
|
Cured (n, %) |
26 (2.4%) |
Improvement |
998 (91.1%) |
Remission |
11 (1.0%) |
No change |
43 (3.9%) |
Worsening |
0 (0.0%) |
Death |
7 (0.6%) |
Death by other diseases |
4 (0.4%) |
Others |
7 (0.6%) |
Length of hospital stay (Mean ± SD) |
24.84 ± 12.25 |
Length of hospital stay (Range, Q1, Q3) |
6–95, 16, 30 |
Complications (n = 1,096) |
|
Postoperative peritonitis |
10 (0.9%) |
Postoperative ileus |
27 (2.5%) |
Additional treatment (n = 1,096) (n, %) |
|
Intravenous injection |
35 (3.2%) |
Radiotherapy |
29 (2.6%) |
Chemotherapy |
2 (0.2%) |
Pairwise comparison between the groups exhibiting the two complications, namely postoperative peritonitis and postoperative ileus, shows that the LOS average was significantly longer in the positive group than in the negative group (Table 2).
Table 2: Descriptive statistics of the length of hospital stay by the occurrence group of their complications
Variables of complications |
Positive |
Negative |
|
|
|
n |
length of hospital stays (1) |
n |
length of hospital stays (1) |
P |
|
|
Postoperative peritonitis |
10 |
38.90 ± 17.65 |
1086 |
24.71 ± 12.11 |
0.000 |
*** |
(2) |
Postoperative ileus |
27 |
35.00 ± 13.19 |
1069 |
24.59 ± 12.11 |
0.000 |
*** |
(3) |
(1) Mean ± SD, (2) Levene’s test, (3) Welch's t-test |
|
|
|
|
|
The two complications were analysed to estimate their effects on the LOS. The resulting estimation formula was obtained by stepwise multiple regression:
lnDi=2.993+0.104A+0.102S3+0.204S4+0.530PP+0.416PI+0.309RT+εi.
The effects of postoperative peritonitis and postoperative ileus on the LOS are statistically significant. Gender, central intravenous injection, and chemotherapy are excluded from the analysis by stepwise multiple regression. In addition, exponentializing the unstandardized coefficients reveals that the LOS was prolonged by 69.9% in cases of postoperative peritonitis and 51.6% in cases of postoperative ileus (Table 3).
Table 3: Estimated effect of the complications on the length of hospital stay
|
β Coefficient |
Standard Error |
t value |
p value |
|
Intercept |
2.993 |
0.025 |
121.757 |
|
|
≥80 years old dummy |
0.104 |
0.041 |
2.517 |
<0.05 |
** |
Stage III dummy |
0.102 |
0.036 |
2.804 |
<0.01 |
*** |
Stage IV dummy |
0.204 |
0.049 |
4.196 |
<0.01 |
*** |
Postoperative peritonitis dummy |
0.530 |
0.152 |
3.486 |
<0.01 |
*** |
Postoperative ileus dummy |
0.416 |
0.130 |
3.195 |
<0.01 |
*** |
Radiotherapy dummy |
0.309 |
0.108 |
2.868 |
<0.01 |
*** |
***p<.01, **p<.05 |
|
|
|
Adjusted: R2: 0.08 |
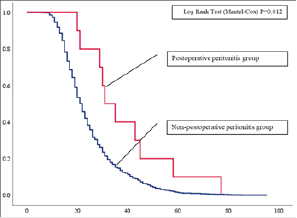
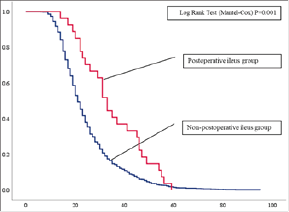
Finally, the cumulative probabilities of hospital stay for patients with and without postoperative peritonitis and postoperative ileus were calculated. The results confirmed that the cumulative probability of hospital stay for the positive group was significantly higher than that of the negative group. The details are as follows:
1. The cumulative probability of hospital stay for the positive group for postoperative peritonitis was 80.0% on the 21st day. This is higher than 50.2% observed in the negative group (80.0%: 27.5% on the 28th day; 40.0%: 15.2% on the 35th day) (Figure 2).
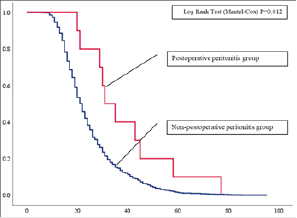
Figure 2: Cumulative probability of hospital stays for postoperative peritonitis
2. The cumulative probability of hospital stay for the positive group for postoperative ileus was 85.2% on the 21st day. This is higher than the 49.6% observed in the negative group (66.7%: 27.0% on the 28th day, 40.7%: 14.8% on the 35th day) (Figure 3).
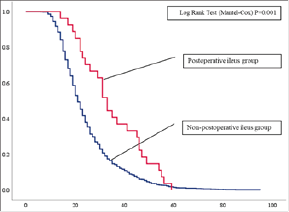
Figure 3: Cumulative probability of hospital stays for postoperative ileus
The data on colon cancer in patients who underwent open colectomy was analysed retrospectively. To establish the relationship between the LOS and the two complications: postoperative peritonitis and postoperative ileus.
The results revealed that the LOS of patients with postoperative peritonitis and postoperative ileus was significantly prolonged by 69.9% and 51.6%, respectively. Moreover, the cumulative probability of hospital stay in the positive group for postoperative peritonitis and postoperative ileus was significantly higher than that in the negative group.
Previous studies have shown that the most frequent postoperative surgical complications observed after colorectal resections were postoperative peritonitis. They are mainly caused by a surgical site infection via anastomotic leakage and postoperative ileus, which can arise from intestinal dyskinesia due to intestinal paralysis or dilation through open surgery. Patients with these complications tend to have a prolonged hospital stay [2-6]. The risk of complications is higher in older patients [10]. Compared with younger patients (≤65 years old; n=211), older patients (>65 years old; n=235) suffer more from ileus, peritonitis or septic shock, pelvic abscesses, and wound infections. The occurrence of postoperative ileus prolonged the patients’ LOS by 29% (n=3,115) [6]. This is like the findings of this study.
Previous studies have not shown a cumulative probability of hospital stay due to complications. As expected, the results of this study showed that the occurrence of postoperative peritonitis and postoperative ileus significantly prolonged the LOS. Patients’ age (≥80 years), severity (pathologic stage III and IV), and receipt of radiotherapy as treatment also prolonged the LOS. The effect was significant (p<0.05, p<0.01, and p<0.01). The findings with respect to age correspond to those of previous studies [2-6, 9-11]. The findings related to age and radiotherapy reflected the clinical features of the patients. These were specified in the DPC/PDPS as the factors that prolonged the LOS. The severity level was determined by the clinical decision of whether surgery was possible. It has also been reported that the prognosis after colectomy was effective even in patients with stage III tumors [9, 10]. However, cancer treatment has been clinically determined in recent years in terms of the survival effect and quality of life (QOL). Therefore, the results of this study may differ from the current clinical judgment.
The results obtained in this study are medically explainable because postoperative peritonitis is mainly caused by surgical site infection and anastomotic leakage [2-6]. Postoperative ileus is primarily caused by intestinal dyskinesia due to intestinal paralysis or dilation through open surgery [2-6]. Although the anastomosis method and the device used during open colectomy have improved, the incidence of complications is still not low [1-4]. Thereby, it must be verified with new data.
Regarding the quality of the surgery, it should be noted that postoperative peritonitis and postoperative ileus prolonged patients’ hospital stay and increased their cumulative probability. A previous study reported several hospital caseloads affected complications, local recurrence, and survival rates [11, 12]. One study showed that low surgery volumes were associated with increased complications, recurrence, and lower survival rates in Norwegian patients with colon cancer (n=3,388). Moreover, patients who underwent surgery in a ‘high-quality hospital’ had a satisfactory prognosis. By contrast, ‘low-quality hospitals’ missed the quality standards of various measures of outcome (anastomotic leakage, postoperative mortality, recurrence, and long-term survival) [11]. In addition, another study showed that the local recurrence rate was 10% among surgeons with a high volume of surgeons, while it was 21% for low volume of surgeons (n=2,815) [12]. These studies implied that surgeons’ experience or volume of surgery in hospitals is the most crucial unit of volume for the prognosis of patients with colon cancer.
If surgeons’ experience or volume of surgery in hospitals contribute to the prognosis of patients, including a shortened LOS, it is necessary to design a framework to enable hospitals to accumulate a higher number of caseloads. Although DPC/PDPS is designed as a medical reward to promote shorter hospital stays, it should ideally promote quality improvement by incorporating ‘quality level of surgeries’ into the medical reward. Consequently, this will encourage surgeons and hospitals to provide high-quality surgeries and perform surgeries aggressively, including perioperative care [13]. If surgeons and hospitals are currently unable to provide high-quality surgeries, they will either avoid performing surgeries or improve the quality of surgeries to perform successful surgeries. Therefore, it is important to set additional rewards for high-quality surgery in medical fee systems to reduce the occurrence of postoperative complications ultimately.
This study had some limitations. First, the outcome of open colectomy may have improved due to introducing a new anastomosis method and device. In such a case, the implications of these results will be weakened. Second, high-quality surgery does not always contribute to the prevention of postoperative peritonitis and postoperative ileus. The risk of surgery is a function of many factors [3], those associated with a patient’s health, such as diabetes mellitus and body mass index [4], and perioperative care, such as that provided by the Surgical Support Team [13]. In addition, there was a lack of indicators to conduct a more accurate analysis. This includes a lack of information on anatomic problems, the American Society of Anaesthesiologists physical status classification, the Clavien-Dindo classification, and surgeons’ experience [13]. Finally, the results cannot be generalized for all population groups in Japan. One criticism may be that the variables in this study were selected according to the hypothesis because it is a retrospective study. However, considering that this study estimated the effects of complications based on data collected from 24 acute care hospitals, the explanatory power of the results is valid. Therefore, it is necessary to re-examine the study variables in the context of Japan’s national data.
This study retrospectively analysed the effects of postoperative peritonitis and postoperative ileus on the LOS of patients who underwent open colectomy. The hospital stays of the positive group pertaining to postoperative peritonitis and postoperative ileus was found to be significantly prolonged compared to that of the negative group. Moreover, the cumulative probability of hospital stay was significantly higher in the positive group than in the negative group.
Directly reducing the risk of postoperative complications requires the design of a framework that encourages quality surgery. If hospitals can charge appropriate fees to reduce the risk of complications, they may spend more on improving medical technology and safety. Therefore, it is important to set additional rewards for high-quality surgery in the DPC/PDPS to reduce postoperative complications.
a The details were as follows: postoperative ileus, 0.993; postoperative peritonitis, 0.747.
- Law WL., Choi HK., Lee YM (2007) The impact of postoperative complications on long-term outcomes following curative resection for colorectal cancer. Annals of Surgical Oncology 14: 2559-2566. [Crossref]
- Dindo D., Demartines N., Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Annals of Surgery 240: 205-213. [Crossref]
- Kirchhoff P., Clavien PA., Hahnloser D (2010) Complications in colorectal surgery: risk factors and preventive strategies. Patient Safety in Surgery 4: 5. [Crossref]
- Scarborough JE., Schumacher J., Kent KC (2017) Associations of specific postoperative complications with outcomes after elective colon resection: a procedure-targeted approach toward surgical quality improvement. JAMA Surgery 152: e164681. [Crossref]
- Deierhoi RJ., Dawes LG., Vick C (2013) Choice of intravenous antibiotic prophylaxis for colorectal surgery does matter. J Am Coll Surg 217: 763–769. [Crossref]
- Iyer S., Saunders WB., Stemkowski S (2009) Economic burden of postoperative ileus associated with colectomy in the United States. J Manag Care Pharm 15: 485-494. [Crossref]
- Japanese Society for Cancer of the Colon and Rectum (2005) JSCCR Guidelines 2005 for the Treatment of Colorectal Cancer. Kanehara & Co., Ltd (in Japanese).
- Japanese Society for Cancer of the Colon and Rectum (2019) JSCCR Guidelines 2019 for the Treatment of Colorectal Cancer. Kanehara & Co., Ltd (in Japanese).
- Neuman HB., Weiss JM., Leverson G (2013) Predictors of short-term postoperative survival after elective colectomy in colon cancer patients ≥80 years of age. Annals of Surgical Oncology 20: 1427–1435. [Crossref]
- Grosso G., Biondi A., Marventano S (2012) Major postoperative complications and survival for colon cancer elderly patients. BMC Surgery 12: S20. [Crossref]
- Wibe A., Eriksen MT., Syse A (2005) Effect of hospital caseload on long-term outcome after standardization of rectal cancer surgery at a national level. British Journal of Surgery 92: 217–224. [Crossref]
- Schrag D., Panageas KS., Riedel E (2002) Hospital and surgeon procedure volume as predictors of outcome following rectal cancer resection. Annals of Surgery 236: 583-592. [Crossref]
- Artinyan A., Nunoo-Mensah JW., Balasubramaniam S (2008) Prolonged postoperative ileus-definition, risk factors, and predictors after surgery. World Journal of Surgery 32: 1495-1500. [Crossref]