Goodpasture's syndrome (GPS) remains a very rare disease entity in the pediatric population characterized by the presence of pulmonary hemorrhage and rapidly evolving glomerulonephritis. Without any appropriate treatment, the disease is generally fulminant and patient and kidney survival is poor. We hereby describe the case of a 15-year-old boy who presented as an early symptom poorly tolerated anemia, with normal renal function and no oliguria nor respiratory symptoms. Past medical history was significant with an episode of transfusion on severe anemia and taking corticosteroids for pneumonia. Bronchoscopy revealed pulmonary hemorrhage and the diagnosis was confirmed by histological exam after kidney biopsy. He was treated with corticosteroids and cyclophosphamide, with a positive response to treatment. He is currently in a stable condition.
Anemia; Goodpasture Syndrome; Pulmonary Hemorrhage; Hematuria; Children
Goodpasture’s disease is an uncommon composite of features including renal failure with pulmonary hemorrhage secondary to an autoimmune response that specifically targets these organ systems. The disease was first described by the American pathologist Ernest Goodpasture in 1919 and was later named after him [1].
Delay in diagnosis and initiating treatment, together with technical difficulties in treatment, can result in failure to halt the progress of the disease and in permanent loss of renal function. The reverse is true with early diagnosis and prompt, aggressive treatment [2].
This case review focuses on the atypical clinical presentation of anti-GBM disease with supporting histologic and radiologic evidence
A 15-year-old Moroccan boy presented loss of appetite, fatigue, palor and mild breath shortage for 1 week.
On admission, examination revealed a pale child with blood pressure of 125/71 mm Hg. He was apyretic, tachycardic, and saturating at 100% at ambient air. The lungs were clear to auscultation. Cardiac examination showed no abnormality. His abdomen was supple and non-tender with no organomegaly. His extremities showed no evidence of edema. Neurologic examination was normal.
Past medical history was significant for an admission about 9 months back with poorly tolerated anemia. Labs at that time were significant for severe anemia (Hb 6.9 g/dl) and iron deficiency. He received two units of whole blood transfusion. 3 months later, he was diagnosed with pneumonia and received antibiotics and corticosteroids. There was no past or family history of renal disease.
Work-up during this current admission confirmed anemia (Hb 7.6g/dl) with a slightly elevated white blood cell count (12,400/mm3) and platelet count (234,000/mm3). Laboratory investigations also revealed microscopic hematuria, proteinuria (2 g/day), Urine output was around 1500 mL/day of normally coloured urine, normal renal function and without hydro electrolyte disturbance.
Anti-nuclear antibodies and antiDNA were negative and rheumatoid factor test was also negative.
A chest X-ray revealed diffuse bilateral interstitial prominence (figure 1). Chest computed tomography realized after 5 days was normal.

Figure 1. Chest X-ray, Diffuse Bilateral Interstitial Prominence
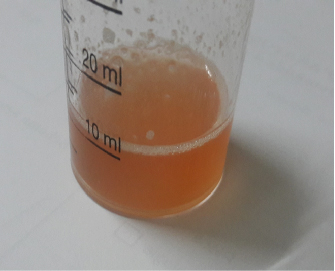
Subsequently, the patient received bronchoscopy. Bronchoalveolar lavage showed alveolar hemorrhage (figure 2) rich in Siderophage with an estimated gold score of 93 corresponding to high resorption.
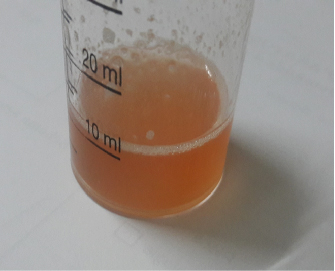
Figure 2. Bronchoscopy Demonstrated Hemorrhagic Bronchoalveolar Lavage
The patient underwent a kidney biopsy and histopathological examination revealed lesions of necrotizing glomerulonephritis with extracapillary segmental proliferative pauci-immune, and IgG linear deposits of the GBM with IF.
Therapy with prednisone, cyclophosphamide was initiated and the patient showed clinical improvement. Finally, he was discharged home with a slow tapering dose of prednisone and cyclophosphamide. Upon discharge the patient was schedule for a monthly follow up.
GPS is a rare condition occurring in approximately 0.5 to 1 per million per year in adults and even more rare in children [3]. The disease predominantly affects the white population, with bimodal age distribution in 20-30 years and 60-70 years old. GPS is rare in children, with only about 30 cases being reported in the pediatric literature, with the youngest reported child being 11 months of age [4].
The etiology of Goodpasture's Syndrome remains unknown. Exposure to environmental factors such as viral infections, hydrocarbons and tobacco may precipitate the disease and worsen the pulmonary lesions [5], these factors were not found during anamnesis of our patient.
Initial presentation of GPS can be nonspecific and often consists of symptoms such as malaise, weight loss, fever, and arthralgia [6]. Kidney disease may occur independently or with pulmonary disease. Pulmonary symptoms may precede renal symptoms by weeks to months with hemoptysis being the most common pulmonary manifestation.
In hindsight, our patient’s initial presentation with anemia was most likely an occult pulmonary hemorrhage and his response to steroids during the second admission has probably slowed the evolution of this disease.
Chest X-ray may be normal in 22% cases. CT chest findings include ground glass opacities, alveolar infiltrates, and consolidations. Radiologic resolution may be seen after 3 and 4 days if the hemorrhage ceases [7].
The diagnosis of antiglomerular basement membrane disease is reliant on detection of anti-GBM antibodies either in circulation or in the tissue by means of renal or pulmonary biopsies. [4]
Without proper management, the shortterm renal prognosis is generally very guarded. Classic therapeutics in the pediatric population is extrapolated from adult guidelines and mostly consists of plasma exchanges associated with immunosuppressive drugs (steroids and cyclophosphamide) [8].
GPS is a rare but serious disease that may occur in adolescents and this diagnosis should be considered even in the absence of characteristic pneumo-renal symptoms. We report a case of a 15-year-old boy who presented with this condition and the difficulties involved in coming to an accurate diagnosis. In hindsight, his initial presentation with severe anemia and iron deficiency was likely an occult pulmonary hemorrhage. His response to steroids during his second admission likely constituted a partial treatment. GPS though rare should be evoke in front unexplained anemia and/or blood streaked sputum in combination with macroscopic or microscopic hematuria. Early diagnosis and intervention are essential for a favorable outcome.
The authors declare that they have no competing interests.
M. Oudrhiri wrote the manuscript. All authors read and approved the final manuscript.
NA
I have no relevant financial interests in this manuscript.
The authors declare that data supporting the findings of this study are available within the article.
Written informed consent was obtained from the patient’s next of kin for publication of this case report and any accompanying images.
- Goodpasture EW (1919) The significance of certain pulmonary lesions in relation to the etiology of influenza. Am J Med Sci 158: 863-870. [Crossref]
- Dixit M P, Kirschner R, Bulimbasic S, et al. (2010) Rescue of renal function in a 3-year-old girl with Goodpasture’s syndrome with a brief review of literature. NDT plus 3: 483-486. [Crossref]
- Fischer EG, Lager DJ (2006) Anti-glomerular basement membrane glomerulonephritis: a morphologic study of 80 cases. Am J Clin Pathol 125: 445-450. [Crossref]
- Master Sankar Raj V, Warnecke D, Roberts J et al. (2017) Antiglomerular Basement Membrane Disease in a Pediatric Patient: A Case Report and Review of the Literature. Case Rep Nephrol. [Crossref]
- Salam N, Rezki H, Fadili W, et al. (2007) Goodpasture's syndrome - Four Case Reports. Saudi J Kidney Dis Transpl 18: 235-238. [Crossref]
- Dammacco F, Battaglia S, Gesualdo L, et al. (2013) Goodpasture's disease: a report of ten cases and a review of the literature. Autoimmunity Reviews 12: 1101-1108.
- Saladi L, Shaikh D, Saad M, et al. (2018) Pulmonary renal syndrome: A case report of diffuse alveolar hemorrhage in association with ANCA negative pauci-immune glomerulonephritis. Medicine 97: e10954. [Crossref]
- Dorval G, Lion M, Guérin S, et al. (2017) Immunoadsorption in anti-GBM glomerulonephritis: Case report in a child and literature review. Pediatrics 140: e20161733. [Crossref]