Background: Woven-like arteries represent a rare congenital vascular variation with only a handful of cases documenting for coronary arteries. The standard diagnostic approach employs angiographic imaging. This vascular anomaly often mimics other vascular diseases, such as stenosis, dissection, or recanalization following a thrombotic occlusion. Accurate differential diagnosis of such woven-like lesions plays an important role in defining treatment strategies.
Case presentation: A 62-year-old female presented with intermittent numbness and weakness on her right side. She was diagnosed with transient ischemic attack, which was associated with woven-like changes in the ipsilateral internal carotid artery revealed by cerebral angiography. Following the diagnosis, the patient was started on secondary preventative strategy to mitigate the risk of an ischemic stroke. Over a follow-up period of 2 years, the patient showed no significant signs of a cerebrovascular event.
Conclusions: To our knowledge, this case presents the first recorded instance of a woven-like change in the internal carotid artery. Identification of this rare vascular anomaly is of great clinical significance. This case underscores the importance of including rare vascular variations in the differential diagnosis to help make effective and personalized patient management choices.
Woven-like vessel; Internal carotid artery; Cerebral angiography; High-resolution magnetic resonance vessel wall imaging; Transient ischemic attack
Abbreviations
ICA: Internal Carotid Artery; TIA: Transient Ischemic Attack; MRA: Magnetic Resonance Angiography; CTP: Computed Tomography Perfusion; DSA: Digital Subtraction Angiography; HRMR-VWI: High-Resolution Magnetic Resonance Vessel Wall Imaging; IVUS: Intravascular Ultrasound; OCT: Optical Coherence Tomography.
A woven vessel observed in coronary angiography was first described by Sane in 1988 and is characterized by the division of the artery into several thin channels and twisting of these channels along the vessel axis that merge again into the distal lumen [1]. It is a rare congenital vascular anomaly that is usually considered benign; however, the etiology and pathogenesis of this anomaly remain unclear [2]. Angiography is used as the diagnostic modality to visualize the woven-like artery [3]. However, this angiographic characteristic may be confused with stenosis, dissection, or recanalized thrombus occlusion. Consequently, unnecessary endovascular treatments may be performed, placing the patient at an increased risk of vascular damage and other complications. Hence, the accurate identification of this vascular variation is important for treatment strategies. Apart from a few individual cases of woven coronary arteries, woven-like changes involving other vessels have not been reported. In this report, to our knowledge, we describe the first case of a 62-year-old female with woven-like Internal Carotid Artery (ICA) associated with a Transient Ischemic Attack (TIA) and review the relevant literature, which might contribute to improving the understanding of this rare anomaly.
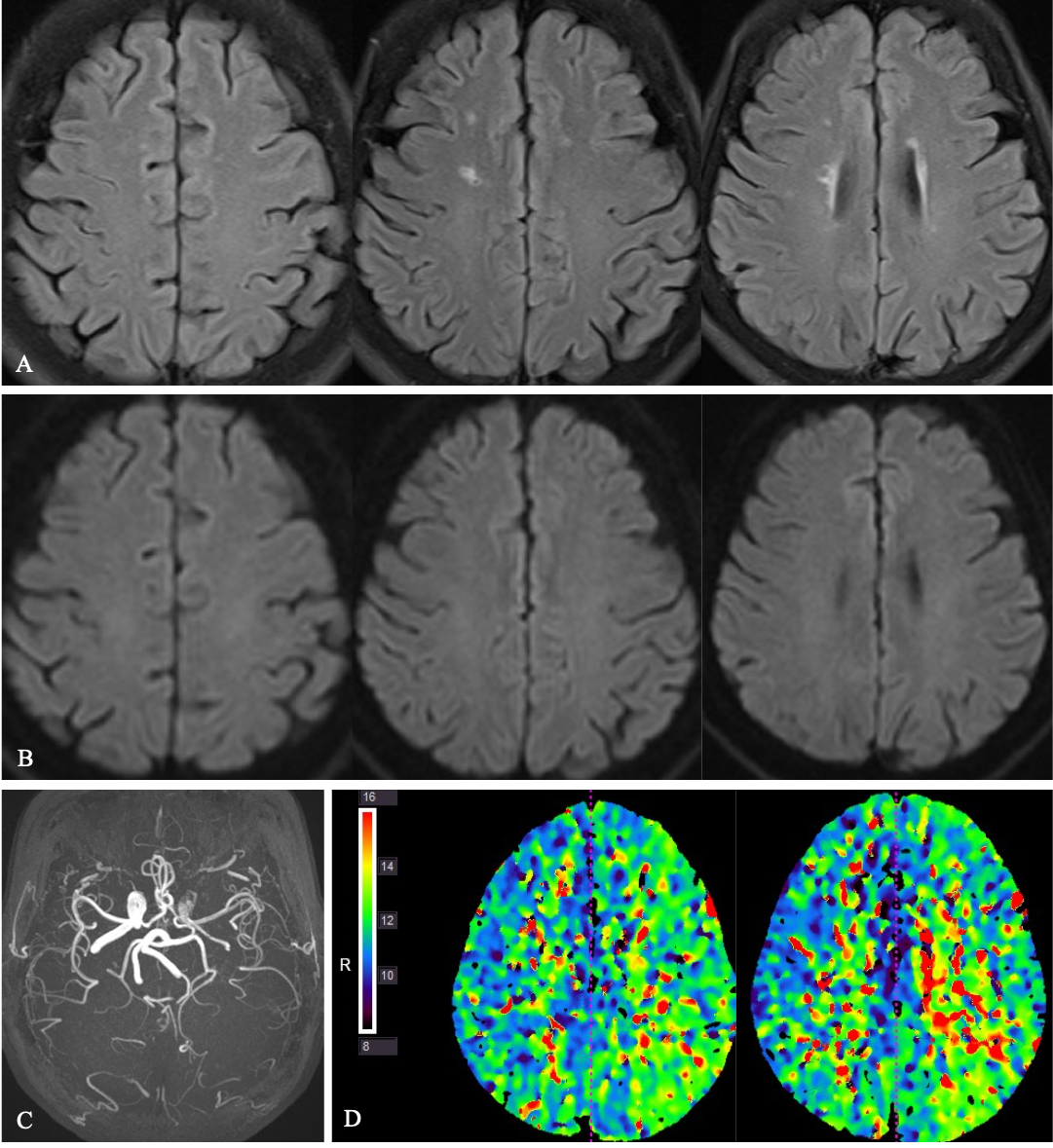
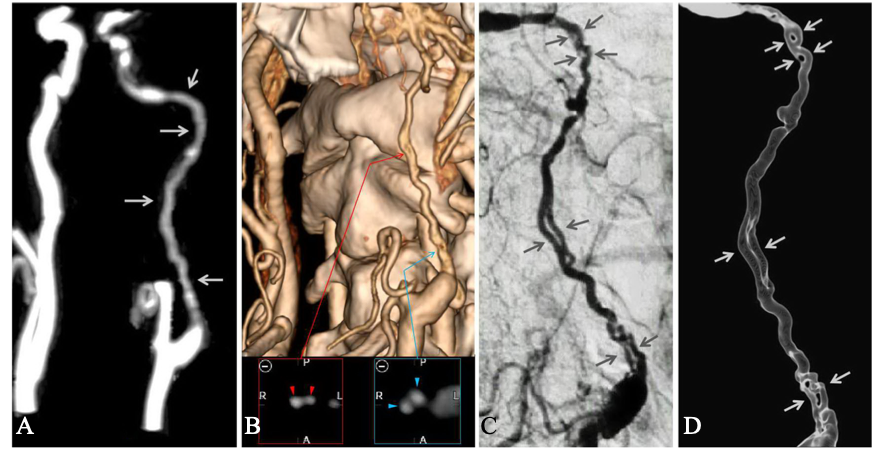
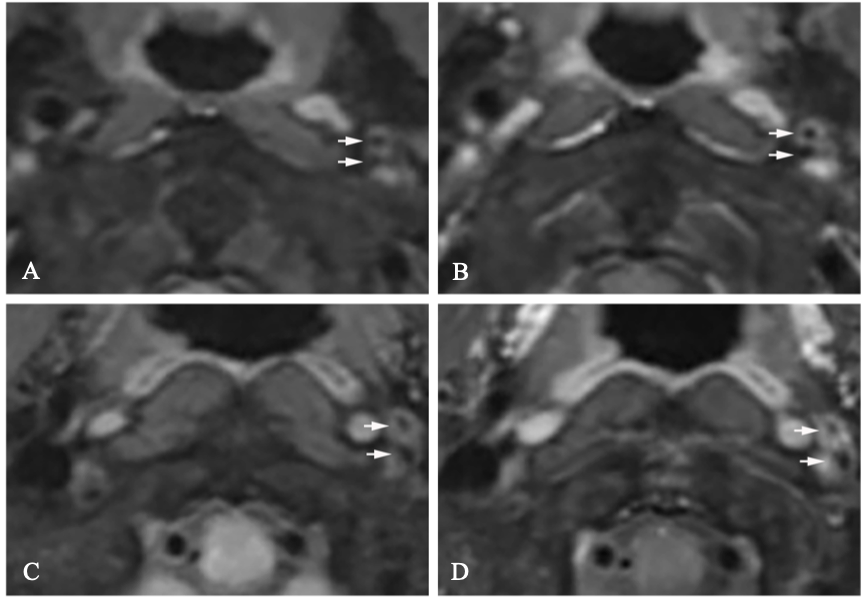
A 62-year-old Chinese female of Han nationality experienced sudden numbness and fatigue in her right limb prior to her admission. These symptoms persisted for 4 hours before resolving completely. The patient had a known history of hypertension for the last 10 years, managed with irbesartan capsules (150 mg once daily). Upon admission, a physical examination was performed, and the results were unremarkable. Biochemical assessment revealed the following abnormal values: erythrocyte sedimentation rate, 45 mm/h. Other routine laboratory tests, such as blood lipids, liver and kidney function, rheumatism, vasculitis, and thrombosis screening, revealed no abnormalities. Echocardiography revealed no significant abnormality. Brain magnetic resonance imaging revealed ischemic foci in the right corona radiate and the regions adjacent to the bilateral ventricles. (Figure 1A); however, diffusion-weighted imaging showed no signs of an acute infarction (Figure 1B). Brain MRA revealed normal intracranial vessels (Figure 1C). Head CTP revealed prolonged time-to-peak in the left frontal and parietal lobes (Figure 1D). Cervical MRA revealed irregular and diffuse stenosis in the cervical and petrous segments of the left ICA (Figure 2A). Cervical computed tomography angiography revealed two double-lumen vessels in the extracranial segment of the left ICA (Figure 2B). To confirm the abnormal changes, two-dimensional and three-dimensional digital subtraction angiography (DSA) were performed. Angiography revealed that the cervical and petrous segments of the left ICA were divided into two thin twisting channels. Through the cervical course, these vessels were intertwined, independent, and then, merged again into the distal lumen in the petrous segment. (Figure 2C and 2D). The features of this anomalous vessel are similar to the typical angiographic findings of a woven coronary artery. Cervical HRMR-VWI revealed a complete wall and lumen structure composing these thin channels in the proximal and middle C1 segments of the left ICA (Figure 3). A woven-like ICA anomaly with TIA was diagnosed. The patient was treated with aspirin (100 mg once daily), clopidogrel (75 mg once daily), atorvastatin (20 mg once daily), and irbesartan hydrochlorothiazide (1 tablet once daily). She did not experience any cerebrovascular events during the 2-year follow-up period.
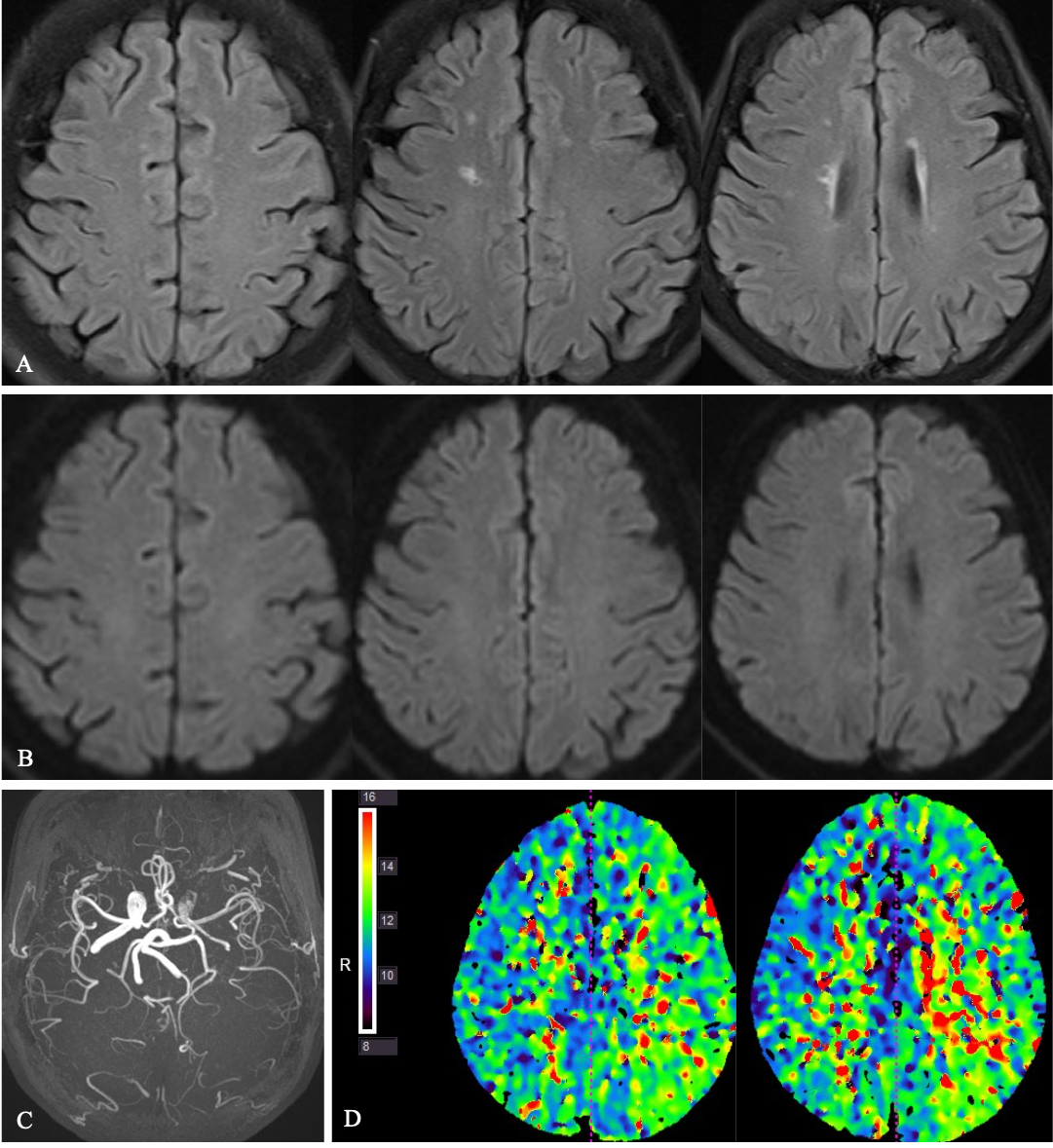
Figure 1: Brain magnetic resonance imaging and computer tomography perfusion imaging. (A) Brain magnetic resonance imaging revealing ischemic foci in the right corona radiata and the regions adjacent to the bilateral ventricles; (B) Diffusion-weighted imaging revealed no acute infarctions; (C) Magnetic resonance angiogram revealed normal intracranial vessels; (D) The head computed tomographic perfusion indicating the prolonged time-to-peak in the left frontal and parietal lobes.
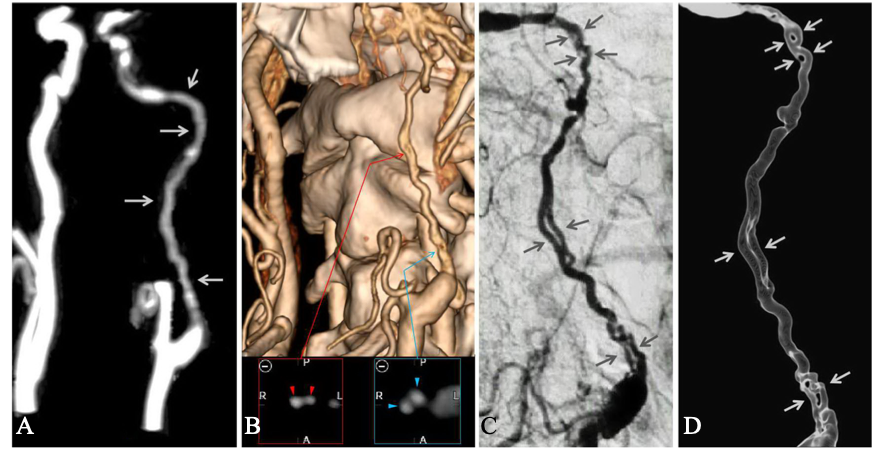
Figure 2: Multiple cervical angiography imaging. (A) Brain magnetic resonance angiogram showing an irregular diffuse stenosis in the cervical and petrous segments of the internal carotid artery (ICA) (arrow); (B) Computed tomographic angiogram showing a double-lumen appears at two sites on the left extra cranial ICA (arrowhead); (C,D) Two-dimensional and three-dimensional digital subtraction angiography revealing that the cervical and petrous segments of the left ICA were divided into two thin twisting channels that merged again into the distal lumen (arrow).
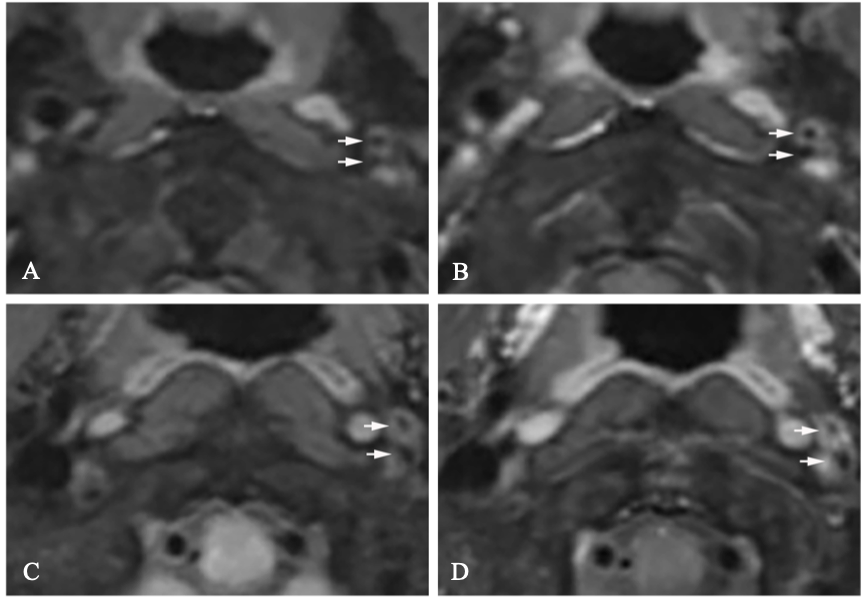
Figure 3: Cervical vessel wall high-resolution magnetic resonance angiogram. (A,B) Cervical high-resolution magnetic resonance vessel wall imaging (HRMR-VWI) revealing complete wall and lumen structure in these thin channels of the proximal and middle C1 segments of the left internal carotid artery (arrowhead); (C,D) Contrast-enhanced cervical HRMR-VWI showing slight and homogenous enhancement in these small vessels (arrowhead).
A typical woven artery is characterized by the separation of the artery into several thin channels that twist along the arterial axis and later re-merge at the distal lumen [3]. Sane initially identified this vascular anomaly in coronary angiography [1]. However, the etiology of the woven-like artery remains unknown. Given that most cases did not result in adverse clinical outcomes and the youngest patient was a 9-month-old child with Kawasaki disease, this vascular abnormality is considered a rare congenital anomaly [4]. To date, individual case reports of this vascular variation have only been described for the coronary artery. To our knowledge, this is the first report documenting a woven-like artery in a vessel other than the coronary artery, suggesting that this pathology can occur in other arteries.
Due to its rarity, woven arteries lack established diagnostic criteria and diagnosis relies predominantly on angiography. A woven artery diagnosis is made when angiography reveals a proximal artery dividing into thin channels, which then re-merge into the distal lumen [5]. In this case, both two-dimensional and three-dimensional DSA revealed that the proximal end of the left ICA divided into small branches. These branches twisted along the arterial axis and converged into the distal vessel. This pattern reappeared near the petrous segment of the left ICA, aligning with the contemporary diagnostic criteria for woven arteries. As histopathological studies have shown that the lumen of these woven-like arteries share an elastic tunica and an endothelial layer [6], some authors have suggested the use of IVUS and OCT as adjunctive tools to observe the vessel wall structure, thus bolstering the diagnostic precision for woven arteries [7,8]. Unfortunately, the patient refused to undergo IVUS or OCT; therefore, multimodal imaging techniques including HRMR-VWI, CTA, and DSA were used to observe the woven-like vessels. This revealed that the separate vessels had a complete wall and lumen structure, which further confirmed the accuracy of the diagnosis.
It is worth noting that a woven artery anomaly may be misinterpreted as a spontaneous dissection or sinus-like bridging collaterals post-chronic thrombotic occlusion recanalization. Consequently, differential diagnosis of woven arteries is vital for making treatment decisions. Because of the intimal tearing of the artery, spontaneous dissection may result in the formation of true lumen and pseudolumen that merged into the same distal access. However, neither a double-lumen sign nor an intimal flap was observed on DSA and no intramural hematoma was found on HRMR-VWI. These signs indicative of a dissection, did not exist in our case [9,10]. Typically, most cases of thrombotic recanalization show it occurs in a local or short vascular lesion [11], but our case demonstrated three woven-like changes in a long artery segment. Additionally, the angiographic morphology beyond the three lesions were normal, distinct from that observed in recanalization after thrombotic occlusion. Moreover, thrombotic recanalization is essentially the development of sinusoidal channels after neovascularization in the thrombus, which is an entity that includes all sinuses with shared vascular access [11]. However, there were no signs of a thrombus filling defect on DSA, and HRMR-VWI showed two separate vascular channels with independent vessel wall and lumen without a thrombus-like structure. Therefore, recanalization post-thrombotic occlusion was ruled out.
Most patients with woven coronary arteries are asymptomatic [3,12]. However, an increase in prevalence of woven-like arteries has been observed among individuals with acute coronary syndrome, myocardial infarction, and sudden cardiac death, owing to improvements in diagnostic techniques [6,7,13,14]. In our case, the patient presented with numbness and weakness of the right limb. The DSA revealed the left proximal ICA was thin with woven-like changes. Head CTP showed blood flow velocity in the left frontoparietal lobes was marginally slow. Therefore, we postulate that structural abnormalities of the left ICA led to cerebral hypoperfusion, thereby contributing to the TIA. Overall, it also suggests that woven-like arteries might cause abnormal blood flow and lead to hypoperfusion symptoms in the target organ.
Navigating the vessels of a woven-like artery with a guidewire and catheter presents a significant challenge due to the relatively small diameter. Additionally, as each branch possesses an independent vascular structure, vascular injury and other serious complications may occur when angioplasty is performed, which is a notable challenge for endovascular treatment. Therefore, it is crucial for physicians to recognize this variation for improved management and prevention of adverse vessel related events and unnecessary procedures.
The management of patients with woven-like artery anomaly remains challenging due to the lack of established treatment guidelines and the highly variable clinical presentations [15]. Current therapeutic decisions must be individualized based on comprehensive clinical and radiographic assessments. Follow-up of those patients are crucial to understand the need for intervention; however, here are few studies that reported regular follow-up of the medical therapy patients. Since most cases are usually findings on angiograms, optimized medical therapy has been the treatment of choice [16]. For symptomatic individuals with woven artery anomalies, prophylactic administration of acetylsalicylic acid might represent a reasonable therapeutic option [17].
A woven artery is a rare congenital vascular variation. In addition to the documented instances in coronary arteries, it can manifest in the ICA. Although usually benign, our case demonstrates that a woven-like ICA can lead to neurological deficits. DSA and HRMR-VWI can be used for the differential diagnosis of woven-like ICA. This report highlights the importance of including rare vascular variations in the differential diagnosis to ensure effective and personalized patient management.
We gratefully thank the patient and her families for their trust in our care and their permission for publication.
Ethics approval and consent to participate:
Written informed consent was obtained from the patient for the publication of this case report.
Consent for publication:
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Availability of data and materials:
The original contributions presented in the study are included in the article, further information on the case including diagnostic and therapeutic details can be made available from the corresponding author on request.
Competing interests:
The authors have no competing interests to declare.
No funding was used in the preparation of this case report.
YM and XC: manuscript writing and figure creating. HC and XC: operation. YM: data collecting. XC: review and editing. All authors contributed to the article and approved the submitted version.
- Sane DC, Vidaillet HJ. (1988) "Woven" right coronary artery: a previously undescribed congenital anomaly. Am J Cardiol 61(13):1158.
- Akcay M, Soylu K. (2018) An unusual etiology of ischemic stroke: woven coronary artery anomaly. J Saudi Heart Assoc 30(4):316-318. [Crossref]
- Joseph SC, D'Antoni AV, Tubbs RS, Gielecki J, Loukas M (2016) Woven coronary arteries: a detailed review. Clin Anat 29(4):502-507. [Crossref]
- Yildirim A, Oguz D, Olgunturk R. (2010) Woven right and aneurysmatic left coronary artery associated with Kawasaki Disease in a 9-month-old patient. Cardiol Young 20(3):342-344. [Crossref]
- Gregorini L PR, Pomidossi G, Saino A, Bossi IM, Zanchetti A. (1995) Woven left coronary artery disease. Am J Cardiol 75(4):311-312. [Crossref]
- Val-Bernal JF, Malaxetxebarria S, Gonzalez-Rodilla I, Salas-Garcia M. (2017) Woven coronary artery anomaly presenting as sudden cardiac death. Cardiovasc Pathol 26:7-11. [Crossref]
- Ayhan S, Ozturk S, Tekelioglu UY, Ocak T. (2013) Woven coronary artery anomaly associated with acute coronary syndrome. Int J Angiol 22(1):55-58. [Crossref]
- Uribarri A, Sanz-Ruiz R, Elizaga J, Fernandez-Aviles F. (2013) Pathological insights of a woven coronary artery with optical coherence tomography. Eur Heart J 34(38):3005. [Crossref]
- Debette S, Leys D. (2009) Cervical-artery dissections: predisposing factors, diagnosis, and outcome. Lancet Neurol 8(7):668-678. [Crossref]
- Wu Y, Wu F, Liu Y, Fan Z, Fisher M, Li D, et al. (2019) High-resolution magnetic resonance imaging of cervicocranial artery dissection: imaging features associated with stroke. Stroke 50(11): 3101-3107. [Crossref]
- Xu B, Li C, Guo Y, Xu K, Yang Y, Yu J. (2018) Current understanding of chronic total occlusion of the internal carotid artery. Biomed Rep 8(2):117-125. Epub 20171218. [Crossref]
- Akyuz A, Alpsoy S, Akkoyun DC (2013) Spontaneous coronary artery dissection and woven coronary artery: three cases and a review of the literature. Korean Circ J 43(6):411-415. Epub 20130630. [Crossref]
- Pauwels R, Coeman M, De Beenhouwer T, Kayaert P. (2020) Woven coronary artery and myocardial infarction. Acta Cardiol 75(2): 158-159. [Crossref]
- Wen W, Liu H, Li J, Zhang Q. (2019) Woven-like change following intracoronary thrombosis recanalization: a case report. BMC Cardiovasc Disord 19(1):317. Epub 20191230. [Crossref]
- Guo Y, Han P, Geng X, Zhu H, Zhang F. (2025) Optical coherence tomography-assisted diagnosis and optimal treatment of three patients with woven coronary artery. Cureus 17(3):e80648. [Crossref]
- Dallan LRP, Dallan LAO, Moretti M, Moragas ABC, Dallan LAP, B Jatene F. (2021) Multivessel Woven Coronary Artery Disease. Braz J Cardiovasc Surg 36(6): 825-828. [Crossref]
- Ayhan S, Ozturk S, Tekelioglu UY, Ocak T. (2013) Woven coronary artery anomaly associated with acute coronary syndrome. Int J Angiol 22(1):55-58. [Crossref]