Retrograde urethrography is part of the fluoroscopic studies that should be performed as part of the training of the resident doctor in radiology and urology, in which although there is a description of the technique, errors of anatomical identification, pathologies and image acquisition are made. Therefore, the knowledge of the errors that can appear before, during and in the post-processing of images, helps us to limit or avoid them.
Retrograde urethrography is a special radiological study, which consists of administering water-soluble contrast medium through the urinary meatus to highlight the male urethra and acquire images of it through fluoroscopic equipment. In a large percentage of cases, the study is requested by doctors specializing in urology and can even be carried out in their presence or by themselves, in order to obtain a correct diagnosis, therefore it is essential that the medium radiologist and radiologist technician, especially personnel in training, know the technique and bear in mind the main errors that may occur before acquiring the image, during and in post-processing.
Technically it is known as retrograde since it is in the opposite direction to urination, one of the main indications is the suspicion of urethral stricture and what the treating physician wants to know is the anatomical location of the narrowing. Another indication is the anatomical evaluation to know if there are congenital malformations, mainly in pediatric patients with a history of recurrent urinary infectious processes. There are some special emergency situations, such as in patients with pelvic trauma, when there is a suspicion of urethral injury, in which a urethrography with computed tomography support can be performed.
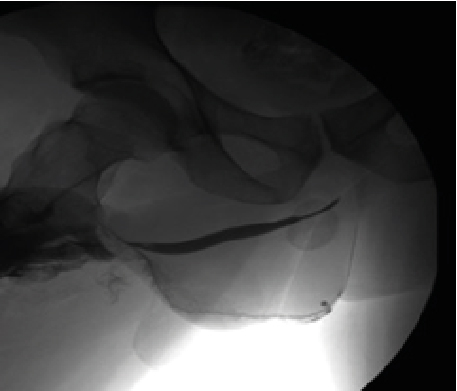
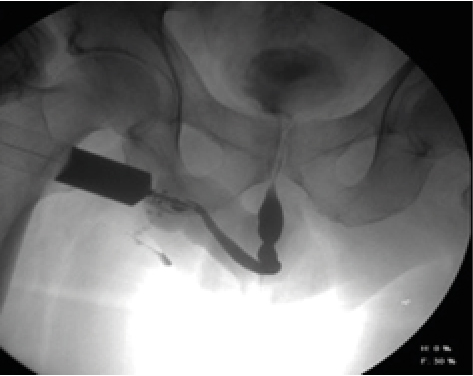
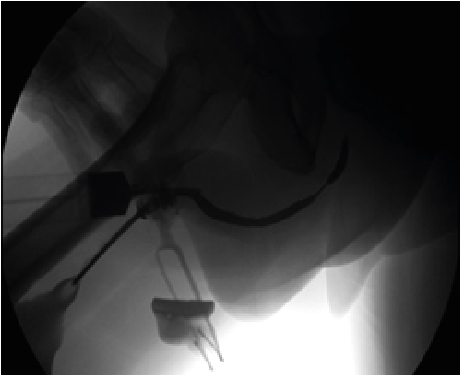
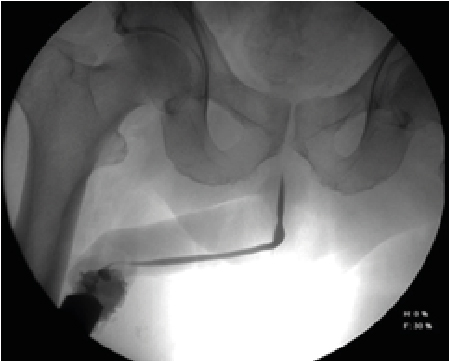
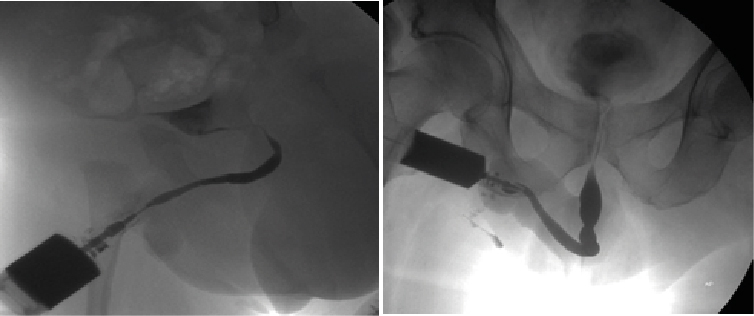
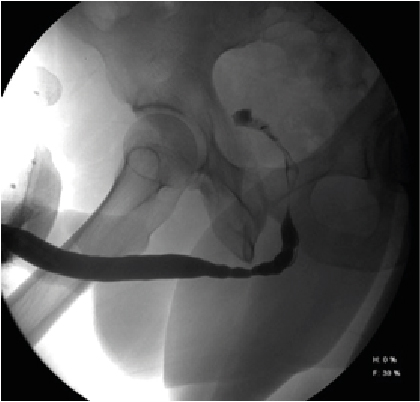
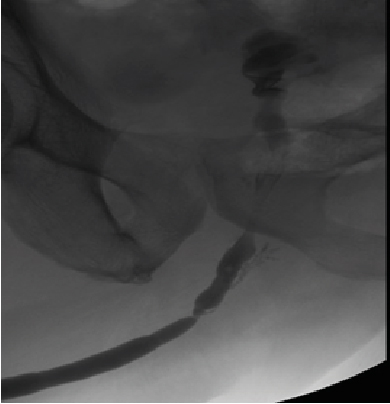
Retrograde urethrography is a very dynamic study, which must be taken into account when acquiring images, especially when sending still images, a common error is the leakage of contrast towards the skin (Figure 1) avoiding using a Foley catheter at the level of distal urethra to retain the contrast, however it can condition trauma [1]. Another common error is the ignorance of ideal projections for evaluation of the urethra (Figure 2), for example the Lauenstein projection, which is more useful for evaluating the hip. The imaging with a lack of contrast between the structures (Figure 3), which can be modified during and after the acquisition. It should be noted that on some occasions, in case of doubt, images will be taken from two different x-ray directions.
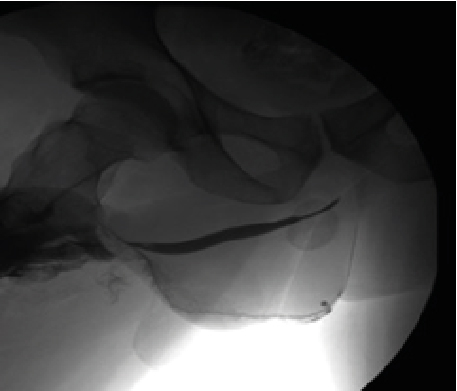
Figure 1: Contrast Drainage in Skin, Can Simulate Double Urethra or False Via
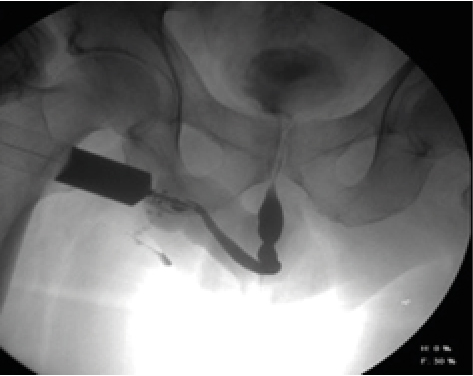
Figure 2: AP Projections with Oblique Taking of the Penis, Avoiding Adequate Visualization of the Urethral Route
Figure 3: Lack of Contrast of the Structures, Either When Acquiring Them and Not Making Adjustments after the Process
In the standard or usual protocol the following steps can be summarized:
- Signing of the informed consent and explanation of the procedure to the patient, as well as the use of protective equipment (apron, gonadal protector, collar and gloves) of the personnel performing the procedure.
- Cleaning the external meatus.
- Placement of a Foley catheter or 16 to 18 Fr catheters.
- If a Foley catheter is used, the balloon is inflated with 1 cc of saline solution.
- Gentle traction of the penis laterally and the patient in a 45º oblique supine position.
- Injection of contrasted material previously diluted to 50 or 60% with continuous and slow pressure as well as use of fluoroscopic guide.
- After filling the anterior urethra, images are acquired when confirming passage of the contrast to the bladder.
- The procedure is terminated, in case of doubts in a suspicious image, it is recommended to repeat the procedure in a different projection.
The same procedure can be repeated by tomography, taking into account the change in dilution to 1:10, to avoid artifacts that prevent the visualization of the urethral anatomy.
An important point to consider prior to its performance is the anamnesis, directed to issues such as allergy to the contrast medium, history of hyperthyroidism and urinary tract infections.
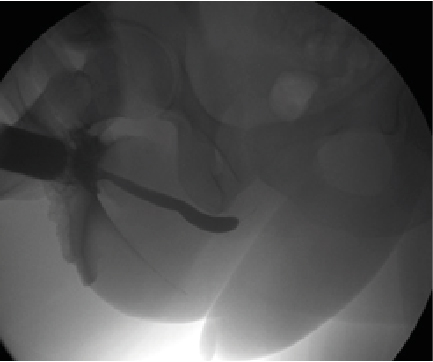
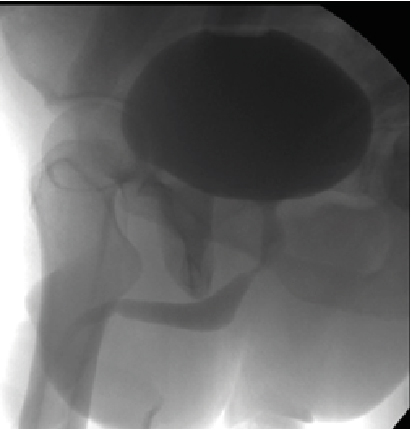
The identification of the anatomical portions of the urethra by retrograde urethrography is part of the learning process of the radiologist technician and medical resident in radiology, which seems easy and yet they are part of daily errors (Figure 4,5,6), it consists the penile urethra, bulbar, bulbomembranous, membranous, urogenital diaphragm, prostatic and verumontanum [2].
The verumontanum or seminal colliculus of the urethra is considered the anatomical landmark at the entrance of the seminal vesicles, being a recess that, as it is not fully distended, can be confused with stenosis [3].
Figure 4: 55-Year-Old Male Who Underwent a Study Due to a Decrease in the Urination Stream, Who Was Described for Prostatic Urethral Stenosis, However After Cystoscopy, the Area of Stenosis Corresponded to the Posterior Bulbar Urethra
Figure 5: 67-Year-Old Man Sent for Difficulty Urinating, Concluding in the Study as Prostatic Urethral Stenosis, However, When Performing a Cystocopy, a Site of Stenosis Was Identified at the Level of the Veru Montanum

Figure 6: 63-Year-Old Male with a History of Prostatic Tran’s Urethral Resection, Which Presented Difficulty in Urination, Was Diagnosed by Image as Posterior Bulbar Stenosis and by Cystoscopy was Anterior Bulbar Urethral Stenosis
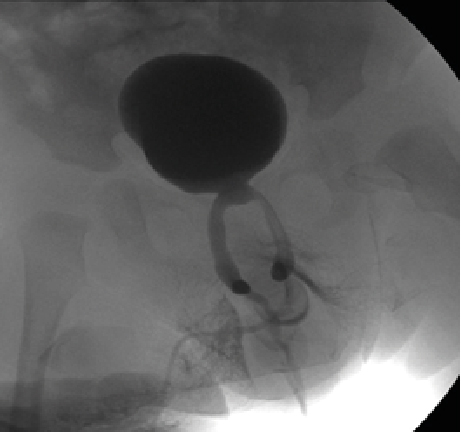
The male urethra has anatomical narrowings such as the vero montanum and the membranous bulb, however, during retrograde urethrography they can be confused with strictures (Figure 7, 8), where we must bear in mind that the stricture can occur at any point along its path and associated to previous surgical events [4].
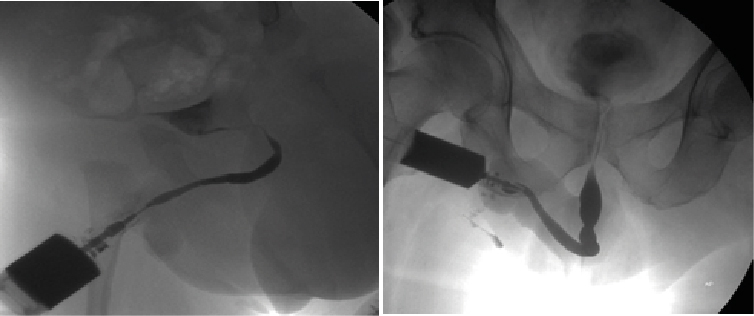
Figure 7: Some of the main errors, is not knowing the normal anatomy to be able to discern between normal and pathological, in these cases of patients of different ages, for example, prostatic stenosis was suspected, however we must bear in mind the presence of the internal and external sphincter, which can prevent the passage of retrograde contrast, which should not be confused with pathological stenosis..
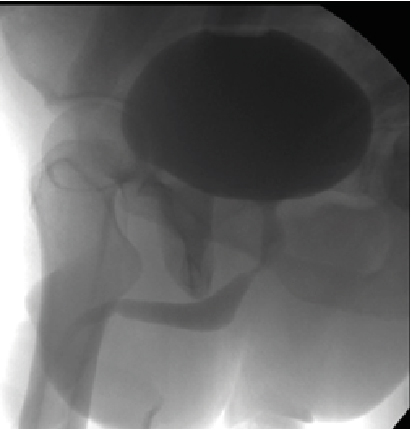
Figure 8:The study of choice if we want to evaluate the real stenosis of the prostatic urethra is cystiscopia and voiding cystography, since in this image the contrast step is adequately identified in the entire urethra, previously diagnosed by retrograde urethrography as prostatic stenosis
Among the findings that we must consider are anatomical variants (Figure 9) such as the presence of a double urethra. For example, we can observe multiple stenoses associated with recurrent infectious processes (Figure 10) or bulbar glands (Figure 11). In the same way, diverticula and urethral calculi should be taken into account.
As part of the protocol, slow distension should be performed to avoid lacerations or injuries due to over-tension [5].
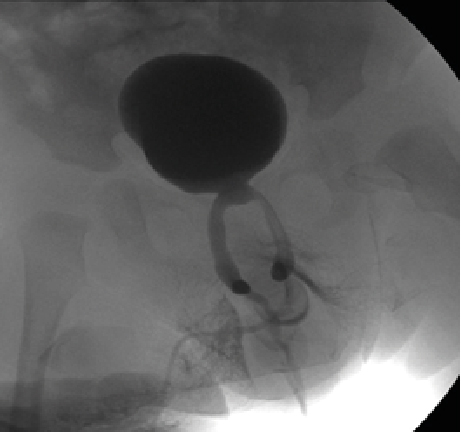
Figure 9: 8-month-old patient, who underwent retrograde urethrography due to difficulty in placing the Foley catheter, suspecting congenital stenosis, finding the presence of a single penile urethra with a double bulbar and prostatic urethra (double arrow), variants to keep in mind so as not to confuse them with false routes
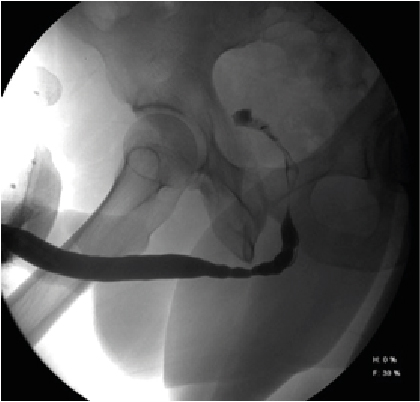
Figure 10: A 16-year-old male with a history of recurrent urinary tract infections, showing fusiform dilations associated with a decrease in urethral diameter, characteristics of multiple stenosis, which should not be confused with filling defects or physiological constriction
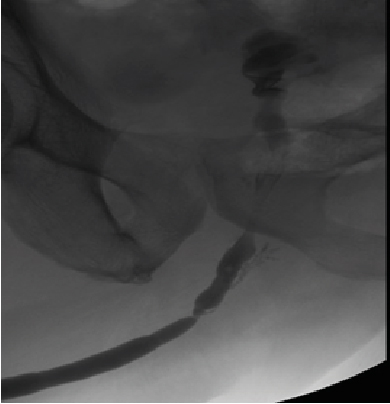
Figure 11: 57-year-old male with post-contrast filling of the urethral bulbous glands, which should not be confused with false via
The study of retrograde urethrography is part of the fluoroscopic studies carried out by resident physicians in training, however the study is completely dynamic and like the dependent operator ultrasound, it is therefore that we must have presents the errors that we can get to commit during its realization and interpretation.
- Juan D Berna Mestre (2009) Urethrography in Men: Conventional Technique versus Clamp Method MD. Randomized Controlled Trial 252: 240-246. [Crossref]
- Jennifer C Flanagan (2018) Urethrography for Assessment of the Adult Male Urethra. Radio Graphics 38: 831-832. [Crossref]
- V Panebianco (2015) Pitfalls in Interpreting mp-MRI of the Prostate: A Pictorial Review with Pathologic Correlation. Insights Imaging 6: 611-630. [Crossref]
- Amsalu Dabela-Biketi (2020) Urethrographic Evaluation of Ana- tomic Findings and Complications after Perineal Masculinization and Phalloplasty in Transgender Patients et al. RadioGraphics 40: 393-402.
- Pietro Pavlica (2003) Imaging of male urethra. Eur.Radiol 13: 1583-1615. [Crossref]